Measuring Scalp Inflammation: How Experts Assess Sensitivity and Healing Progress
Michele Marchand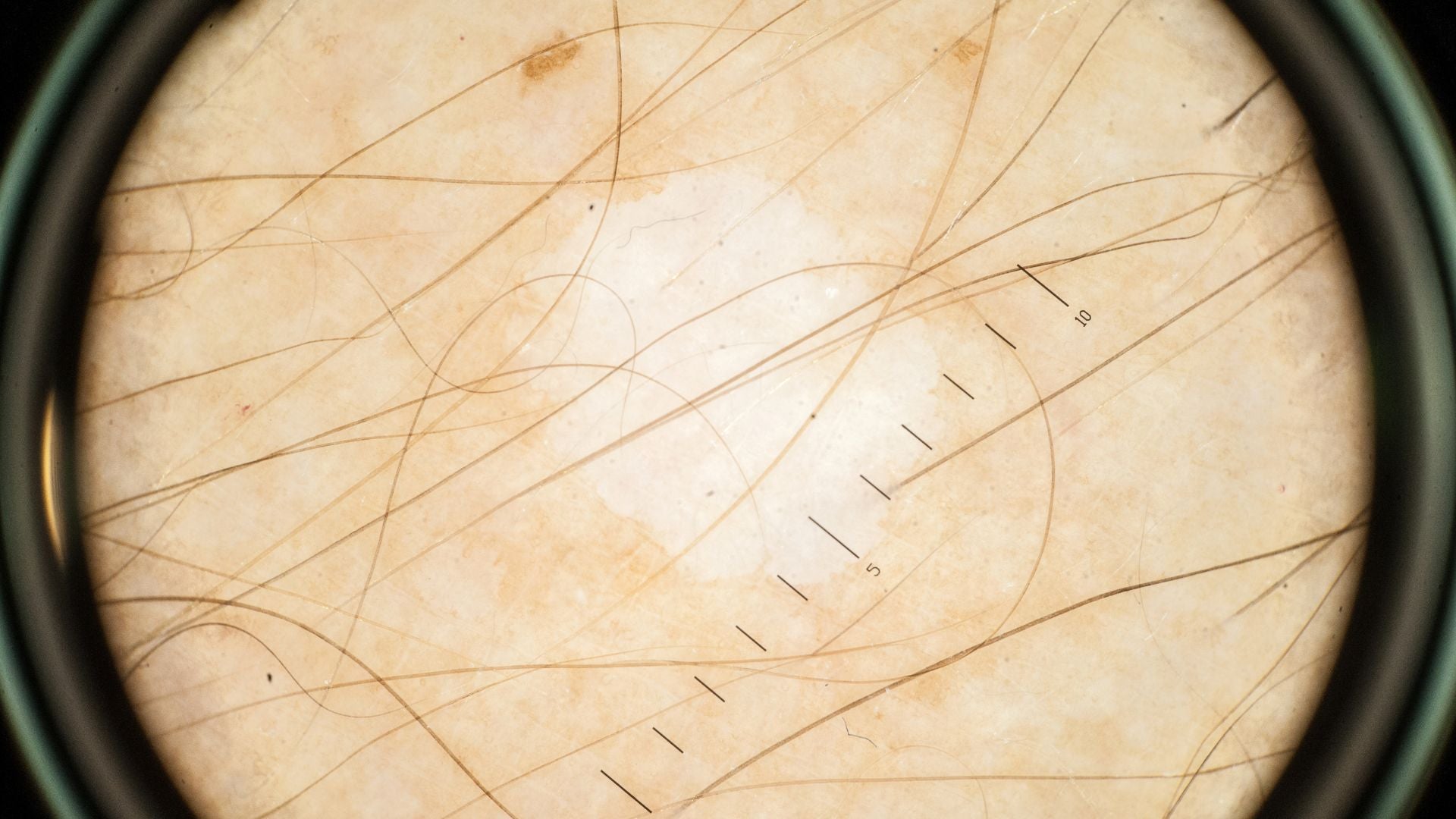
Table of Contents
- How do dermatologists and patients measure scalp inflammation safely and accurately?
- What Is Scalp Inflammation?
- Why Measuring Scalp Inflammation Matters
- Key Metrics Dermatologists Use
- 1. Erythema Index (Redness Measurement)
- 2. Sebum and Hydration Levels
- 3. Transepidermal Water Loss (TEWL)
- 4. Itch and Pain Scales
- 5. Inflammatory Biomarkers (Advanced Testing)
- How to Measure Scalp Inflammation at Home
- Professional Diagnostic Tools
- Understanding Scores and Severity Levels
- How to Track Improvement Over Time
- Gentle Strategies to Support Scalp Recovery
- When to Seek Professional Help
- Glossary
- Claims Registry
How do dermatologists and patients measure scalp inflammation safely and accurately?
Disclaimer: This content is for informational purposes only and is not intended as medical advice. Always consult a qualified dermatologist or healthcare professional for diagnosis and treatment.
What Is Scalp Inflammation?
Scalp inflammation is the body’s immune response to irritation, infection, or injury occurring on the scalp. It often presents as redness, tenderness, itching, or flaking, but in some cases, the symptoms are subtle and progress slowly over time. Medically, inflammation refers to an increase in blood flow and immune cell activity within an area trying to repair itself. On the scalp, this process can involve the tiny follicles that grow each hair strand. When inflammation is persistent, it can lead to follicular damage, causing shedding, thinning, or even permanent hair loss if left untreated¹.
The causes of scalp inflammation vary widely. Common culprits include seborrheic dermatitis (a chronic inflammatory reaction to yeast on the scalp), psoriasis (an autoimmune condition that accelerates skin cell turnover), and allergic contact reactions to ingredients like fragrances or preservatives. The scalp microbiome, the ecosystem of bacteria and fungi that lives on your skin, also plays a key role. When this microbiome becomes imbalanced, inflammation often follows.
Understanding inflammation requires looking beyond visible irritation. Even microinflammation, subtle immune activity occurring below the skin surface, can affect scalp comfort and long-term hair density. Recognizing its signs early allows for gentler, more effective interventions before chronic damage develops.
Why Measuring Scalp Inflammation Matters
Measuring inflammation is not just about diagnosing a problem; it is about understanding its scope and preventing escalation. Many people with sensitive scalps mistake early inflammation for simple dryness or product buildup. But inflammation is dynamic; it changes in intensity and location depending on triggers. Without measurement, you may treat symptoms sporadically, missing the opportunity to calm the underlying cause.
Monitoring inflammation helps in several ways:
-
Identifying triggers and cycles: Keeping track of flare-ups reveals patterns such as irritation after coloring, flare-ups following stress, or weather-related dryness.
-
Evaluating treatment effectiveness: Whether you are using medicated shampoos, barrier creams, or probiotics, having measurable indicators helps determine if your regimen works.
-
Preventing overtreatment: Some people use harsh antifungal or exfoliating products when their scalp is only mildly irritated, which can worsen sensitivity².
-
Supporting medical evaluation: Objective data and consistent tracking help dermatologists tailor treatment plans more precisely.
Inflammation can be both surface-level and deep-rooted. Measuring it systematically ensures you do not overlook the deeper immune activity that could impact long-term scalp health.
Key Metrics Dermatologists Use
Dermatologists rely on both clinical observation and technological tools to assess scalp inflammation accurately. These measurements help quantify redness, hydration, and immune response in ways the naked eye cannot.
1. Erythema Index (Redness Measurement)
Redness, known medically as erythema, is one of the most visible signs of inflammation. Dermatologists measure erythema using colorimetry, a method that quantifies skin redness through reflected light, or trichoscopy, which uses high-magnification imaging to reveal subtle vascular changes beneath the surface³. These tools can identify early inflammation before symptoms intensify. Chronic erythema can signal persistent irritation, often linked to product sensitivity or chronic dermatitis.
2. Sebum and Hydration Levels
Sebum, the scalp’s natural oil, protects the skin and maintains flexibility. Too much sebum can feed microorganisms like Malassezia, a yeast associated with dandruff and irritation. Too little leads to dryness and barrier disruption. Devices such as the Sebumeter and Corneometer measure oil and hydration, providing a baseline for evaluating balance⁴. Balanced readings suggest a healthy scalp barrier, while extreme levels often correlate with inflammation.
3. Transepidermal Water Loss (TEWL)
TEWL measures how quickly water evaporates from the scalp surface. Higher readings indicate that the barrier is compromised, meaning the scalp struggles to retain moisture and defend against irritants. TEWL testing is commonly used in sensitive scalp research, helping identify individuals with impaired skin defenses⁵. A consistently high TEWL reading often predicts chronic sensitivity.
4. Itch and Pain Scales
Even when visible redness is minimal, discomfort can reveal inflammation beneath the surface. Dermatologists use itch (pruritus) and pain intensity scales, where patients rate sensations from 0 (none) to 10 (severe). These scales, when combined with photographic or dermoscopic evidence, create a fuller understanding of inflammation over time.
5. Inflammatory Biomarkers (Advanced Testing)
For complex or resistant cases, clinicians may test for inflammatory biomarkers such as cytokines IL-1α and TNF-α. These proteins act as messengers in the immune system. Elevated levels in scalp tissue or sebum indicate active inflammation⁶. Though not routinely available in all clinics, these biomarkers provide precise insight into the biological processes driving discomfort.
How to Measure Scalp Inflammation at Home
You do not need laboratory equipment to start understanding your scalp. Observation, consistency, and a few affordable tools can offer valuable insights into your scalp’s condition.
1. Visual and Sensory Checks
Stand in natural light or use a handheld mirror to inspect different areas of your scalp. Look for redness, scaling, shiny patches, or small bumps. Lightly press your fingers along the scalp line; warmth or tenderness can signal inflammation. Check behind the ears and nape, where buildup and irritation often start.
2. Itch or Tenderness Diary
Write down your symptoms daily or weekly. Rate itch, pain, or tightness on a 1–10 scale, and note when they appear. Try to link changes to triggers like new shampoos, stressful events, or diet changes. Over time, patterns will emerge that can help you modify habits.
3. pH and Sebum Testing Kits
At-home kits can measure your scalp’s pH and sebum levels. Healthy scalp pH ranges from 4.5 to 5.5. If readings are higher, your barrier may be compromised; if lower, overexfoliation or harsh cleansers may be to blame⁷. Consistent readings outside the normal range often signal inflammation or barrier dysfunction.
4. Scalp Imaging Tools
Affordable smartphone microscopes can magnify the scalp surface up to 200x, revealing fine flakes, blocked follicles, or early redness. Capture photos regularly to track improvement. Even without professional calibration, these images help visualize changes that would otherwise go unnoticed.
Professional Diagnostic Tools
When home observation reveals persistent redness or pain, a professional assessment provides the clarity you need. Dermatologists combine visual inspection with diagnostic technologies to quantify inflammation objectively.
-
Trichoscopy: This non-invasive technique magnifies the scalp up to 100 times, showing follicular openings, microvascular structures, and keratin buildup. It is especially helpful for differentiating between dandruff, psoriasis, and folliculitis.
-
Biopsy: In resistant or unclear cases, a dermatologist may remove a small tissue sample for microscopic analysis. This confirms inflammatory cell types and rules out autoimmune conditions like lupus or lichen planopilaris.
-
AI-Powered Dermoscopy: Modern clinics use artificial intelligence to measure redness intensity, scaling density, and follicle health over time. AI algorithms standardize scoring, reducing human bias.
Professional evaluation ensures that what appears to be inflammation is not an infection or scarring process in disguise.
Understanding Scores and Severity Levels
Inflammation can range from mild irritation to severe immune activity. Dermatologists often categorize it into levels based on both symptoms and objective readings. The following table shows typical thresholds:
| Severity | Redness (Erythema Index) | TEWL (g/m²/h) | Symptoms |
|---|---|---|---|
| Mild | Light pink, localized | <15 | Occasional itch, minor flaking |
| Moderate | Red patches, scattered | 15–25 | Noticeable itch or tenderness |
| Severe | Deep red, widespread | >25 | Burning, soreness, or hair loss |
Understanding where your scalp falls within these categories helps you choose the right care. Mild cases often respond to soothing and barrier-strengthening products, while severe inflammation requires medical-grade anti-inflammatories and possibly prescription antifungal or corticosteroid treatments.
How to Track Improvement Over Time
Tracking is the bridge between awareness and recovery. Consistency, not complexity, matters most. Follow the same observation routine weekly for 8–12 weeks.
Tips for Reliable Tracking:
-
Always inspect your scalp in the same lighting conditions.
-
Part your hair in identical sections for consistent viewing.
-
Take progress photos every two weeks.
-
Record itch, flaking, and pain on a 1–10 scale.
-
Introduce only one new product at a time to isolate effects.
You will know you are improving when redness fades, flaking lessens, and sensations become less intense. Reducing TEWL readings or balanced hydration measurements are also strong indicators of recovery. If no change occurs after a month, seek dermatological guidance; ongoing inflammation may require medical intervention.
Gentle Strategies to Support Scalp Recovery
Measurement is essential, but healing relies on daily care and consistency. The goal is to reduce irritation, restore barrier strength, and calm overactive immune responses.
Recommended Supportive Measures:
-
Cool compresses: Apply a soft, damp cloth for 5–10 minutes to soothe burning or tightness.
-
Fragrance-free cleansing: Use mild shampoos formulated for sensitive scalps containing zinc pyrithione, piroctone olamine, or oat extract.
-
Scalp hydration: Look for products with glycerin, panthenol, or ceramides to restore moisture balance.
-
Anti-inflammatory nutrients: Omega-3 fatty acids (from salmon, chia, or flaxseed) and antioxidants (from berries or green tea) support internal balance.
-
Stress management: Chronic stress elevates cortisol, which can worsen inflammation. Simple mindfulness or breathing techniques can make a difference.
Even gentle routines take time. The scalp renews itself approximately every 28 days, so visible improvements often appear gradually. Think of scalp care as training, not treatment; each week builds resilience.
When to Seek Professional Help
Some inflammation can be self-managed, but there are red flags that call for medical evaluation:
-
Widespread redness that expands or oozes.
-
Burning or pain interfering with daily comfort.
-
Noticeable hair thinning or patchy shedding.
-
Yellow crusts or pustules indicating possible infection.
A dermatologist can confirm whether the inflammation is related to infection, autoimmune disease, or barrier dysfunction. Early consultation reduces risk of scarring and supports long-term scalp and follicle health.
Healing a sensitive scalp is a journey; progress comes from small, consistent steps supported by reliable measurement and compassionate care.
Glossary
- Erythema: Redness caused by increased blood flow during inflammation.
- Transepidermal Water Loss (TEWL): The rate at which water evaporates through the skin barrier, indicating barrier health.
- Trichoscopy: Digital scalp imaging that magnifies follicles and skin structures for diagnosis.
- Cytokines: Immune proteins that act as chemical messengers during inflammation.
- Sebumeter/Corneometer: Devices used to measure scalp oil (sebum) and moisture content.
- Microinflammation: Subtle, often invisible inflammation beneath the skin surface.
- Scalp Barrier: The outer layer of the scalp that locks in moisture and prevents infection.
- Seborrheic Dermatitis: A chronic inflammatory scalp disorder linked to yeast and excess oil.
- Folliculitis: Inflammation of the hair follicle caused by infection or irritation.
- Sensitive Scalp: A scalp prone to redness, itching, or tightness due to barrier weakness or nerve sensitivity.
Claims Registry
| # | Claim | Source | Accessed | Anchor Extract | Notes |
|---|---|---|---|---|---|
| 1 | Persistent inflammation can disrupt hair follicles, leading to shedding. | "Inflammatory hair loss: Pathogenesis and clinical patterns," Trüeb RM, Dermatology, 2015. | 2025-10-27 | "Inflammation within follicular units contributes to hair shedding and miniaturization." | Peer-reviewed dermatology review. |
| 2 | Measuring inflammation helps avoid over- or under-treatment. | American Academy of Dermatology (AAD) Guidelines, 2022. | 2025-10-27 | "Objective assessment reduces misdiagnosis and inappropriate treatment intensity." | Authoritative clinical guideline. |
| 3 | Colorimetry and trichoscopy can detect subclinical scalp redness. | "Noninvasive evaluation of scalp erythema," Lee et al., Skin Research and Technology, 2021. | 2025-10-27 | "Trichoscopy reveals microvascular dilation invisible to the naked eye." | Peer-reviewed imaging study. |
| 4 | Sebumeter and Corneometer measure scalp oil and hydration objectively. | Courage+Khazaka Electronic GmbH, Technical Manual, 2023. | 2025-10-27 | "Sebum and hydration measurement devices for clinical skin and scalp testing." | Manufacturer’s validated instrument data. |
| 5 | TEWL is a key benchmark in sensitive scalp studies. | "Barrier impairment in sensitive scalp," Misery et al., International Journal of Dermatology, 2018. | 2025-10-27 | "TEWL levels correlate with sensitive scalp symptoms and redness." | Clinical dermatology research. |
| 6 | Elevated cytokines indicate ongoing immune activity. | "Cytokine profiles in scalp inflammation," Chen et al., Journal of Inflammation Research, 2020. | 2025-10-27 | "IL-1α and TNF-α levels were elevated in inflamed scalp tissue." | Peer-reviewed study. |
| 7 | Large pH or sebum fluctuations may indicate barrier disruption. | "Scalp pH and microbiome balance," Darlenski et al., Skin Pharmacology and Physiology, 2019. | 2025-10-27 | "Deviations from physiological pH impair barrier integrity and microbial balance." | Clinical research. |




