Patch Testing and Symptom Tracking Protocols for Sensitive Scalp Management
Michele Marchand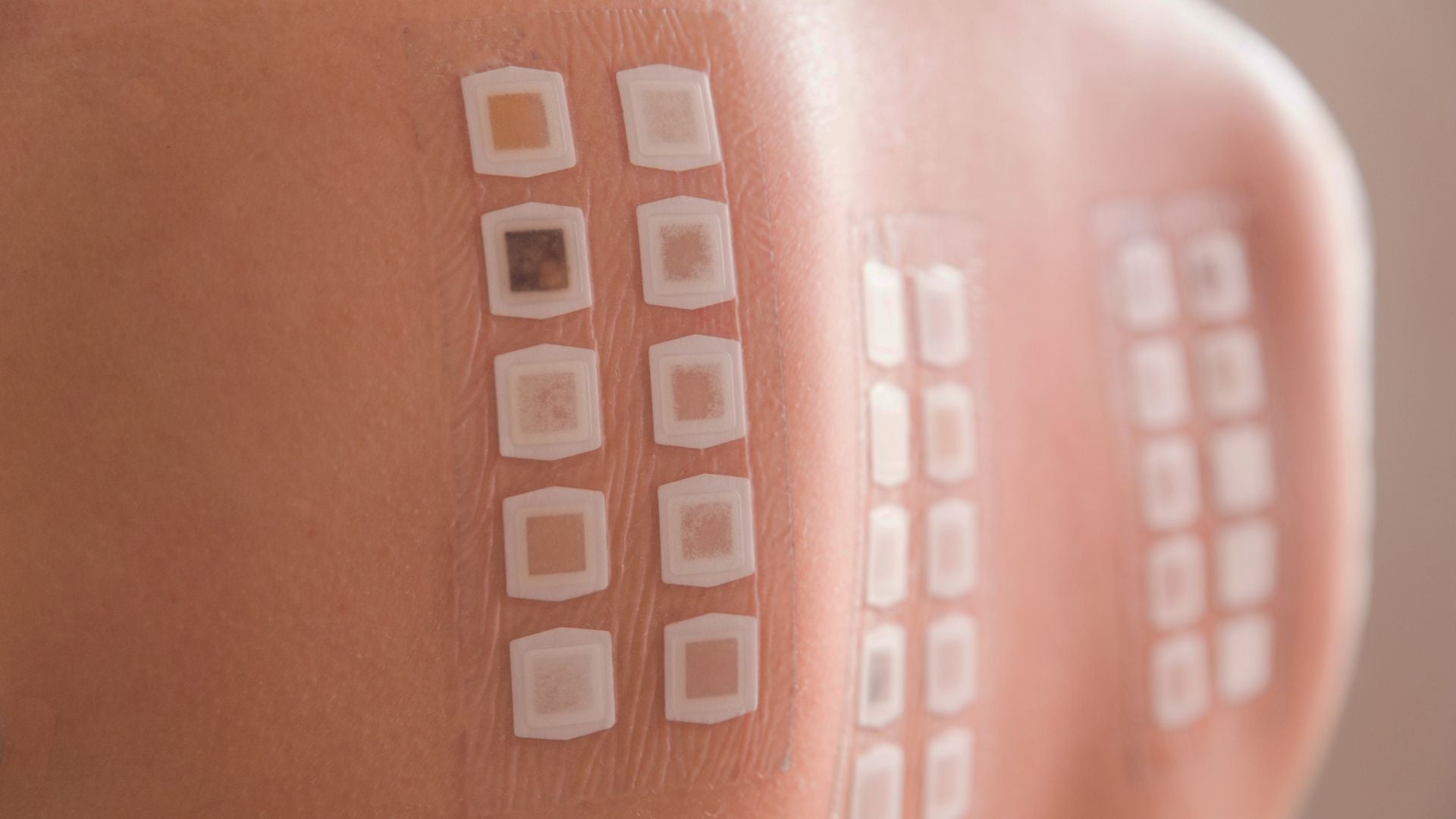
Table of Contents
- Which diagnostic and daily tracking methods best identify allergens and reduce inflammation?
- What Is Patch Testing and Why It Matters for Sensitive Scalps
- Common Scalp Allergens to Know Before Testing
- How to Prepare for a Patch Test
- The Patch Testing Process Step-by-Step
- Creating Your Trigger Tracking Log
- Sample Patch Testing and Tracking Templates
- When to Seek Professional Help
- At-Home Care Between Tests
- How to Discuss Results with Your Dermatologist
- Glossary
- Claims Registry
Which diagnostic and daily tracking methods best identify allergens and reduce inflammation?
Disclaimer: This guide is for educational purposes only and should not replace personalized medical advice. Always consult a qualified dermatologist or healthcare provider for diagnosis and treatment recommendations.
What Is Patch Testing and Why It Matters for Sensitive Scalps
Patch testing is a diagnostic method dermatologists use to identify specific substances that trigger allergic or irritant reactions on the skin. It is one of the most reliable ways to determine why you might be experiencing itching, burning, or inflammation on your scalp. During the procedure, small quantities of suspected allergens such as hair dye ingredients, preservatives, or surfactants are applied to small adhesive chambers placed on the skin, usually the upper back. These chambers remain in place for about 48 hours, allowing the skin to respond naturally.¹
After the test patches are removed, your dermatologist examines each site for redness, swelling, or raised bumps. Because contact allergies often develop slowly, additional readings occur at 72 or even 96 hours after application.² This delay helps capture reactions that take longer to appear, ensuring that no sensitivity goes unnoticed.
For people with sensitive scalps, patch testing is invaluable. Many assume that irritation is caused by stress or poor hygiene, when in fact it often stems from hidden allergens in common hair care products. Identifying the true culprit allows you to eliminate problem ingredients confidently and restore comfort without unnecessary product guessing.
Common Scalp Allergens to Know Before Testing
Understanding what might be irritating your scalp before testing gives you a head start. Many allergens hide in everyday products labeled as “gentle” or “natural.” Recognizing these helps guide your dermatologist toward more precise testing.
Here are some of the most frequent triggers:
-
Paraphenylenediamine (PPD): A powerful dye used in permanent and semi-permanent hair color. It is one of the most common causes of allergic scalp dermatitis.
-
Fragrance mix and balsam of Peru: Fragrance blends are found in everything from shampoos to leave-in conditioners. Even natural essential oils can cause allergic reactions.
-
Methylisothiazolinone (MI) and methylchloroisothiazolinone (MCI): Preservatives that extend product shelf life but are known sensitizers.
-
Nickel or cobalt: Metals sometimes found in product packaging, applicators, or hair clips that come into frequent contact with the scalp.
Identifying these ingredients in your hair care routine helps your dermatologist choose the most relevant allergens for testing.³ It also empowers you to start scanning labels more critically, spotting potential irritants early.
How to Prepare for a Patch Test
A little preparation ensures your test results are accurate and comfortable. Since patch testing involves precise skin responses, even minor disruptions can affect outcomes.
Follow these steps before your appointment:
-
Avoid topical steroids or antihistamines for at least one week, unless otherwise directed. These can suppress skin reactions, leading to false negatives.
-
Bring your everyday hair and scalp products to the clinic. Your dermatologist may apply samples of your own products alongside the standard allergen panels.
-
Plan for several visits across multiple days. Patch tests typically involve application, removal, and follow-up readings to ensure complete interpretation.
-
Wear loose, breathable clothing that allows your back to remain uncovered during application and inspection.
Tip: The day before your appointment, cleanse your skin gently without applying lotions, oils, or perfumes to the area where patches will be placed. Excess oils can interfere with adhesion and accuracy.
Understanding the testing schedule helps you plan work and exercise around it. Heavy sweating, showering, or back washing may dislodge the patches, so many people find it helpful to schedule testing during less physically active weeks.
The Patch Testing Process Step-by-Step
The testing process involves multiple readings because allergic contact dermatitis reactions evolve over time.
-
Application: The dermatologist applies adhesive patches containing small amounts of allergens to your back. Each allergen is labeled and documented for accurate interpretation.
-
Waiting period (48 hours): You’ll be asked to avoid moisture, strenuous activity, and friction. The area may feel mildly itchy, which is normal.
-
First reading (Day 2): After 48 hours, the patches are removed, and early skin changes are recorded.
-
Second reading (Day 3 or 4): A follow-up visit captures delayed responses, which are characteristic of allergic contact dermatitis.
Each reaction is graded using a standardized scale ranging from negative (no reaction) to strong positive (redness, papules, vesicles).⁴ The results are reviewed alongside your exposure history to identify the likely triggers.
Your dermatologist may photograph or document these findings in a patient record to help track long-term sensitivity patterns. This information becomes part of your dermatologic history, guiding future product recommendations and treatment decisions.
Creating Your Trigger Tracking Log
Identifying your allergens is only the beginning. The next step is learning how to manage and avoid them effectively. A trigger tracking log helps capture subtle patterns, like whether symptoms flare during certain weather conditions, hormonal changes, or after switching products.
Recommended columns:
-
Date and time: Record when symptoms appear or worsen.
-
Product used: Include product name, batch number, and whether it’s new or reformulated.
-
Symptom details: Describe itching, redness, tenderness, or flaking in plain language.
-
Environmental factors: Note humidity, stress, diet, or temperature changes.
-
Interventions: Record what you did in response, such as washing your hair, applying a topical, or stopping a product.
By reviewing the log over time, you and your dermatologist can see if certain patterns emerge. For example, a preservative may cause irritation only when combined with heat or sweat, or symptoms might worsen during periods of stress when barrier function weakens.
Tip: Keep digital photos of flare-ups to show changes over time. Even subtle redness can be easier to recognize when compared visually.
Sample Patch Testing and Tracking Templates
Template 1: Patch Testing Results Summary
| Allergen | Source Product | Reaction (+/-) | Notes |
|---|---|---|---|
| PPD | Hair dye | +++ | Strong redness and swelling at 72 hours |
| Fragrance mix | Shampoo | + | Mild itching and pinkness |
| MI/MCI | Conditioner | - | No visible reaction |
| Nickel | Hairpin | ++ | Moderate swelling, localized |
Template 2: Weekly Trigger Tracking Log
| Date | Product | Symptoms | Environment | Intervention |
|---|---|---|---|---|
| Oct 10 | New scalp serum | Mild redness, tingling | Warm, humid weather | Stopped use, washed scalp gently |
| Oct 12 | None | No symptoms | Cloudy, cool | Continued hypoallergenic shampoo |
| Oct 14 | Hair mask | Itching, mild flaking | Stressful day, late wash | Applied colloidal oatmeal mask |
Using these templates consistently can transform trial-and-error into clear, actionable insights. Many patients find that once their personal allergen list is clear, product selection becomes much less stressful.
When to Seek Professional Help
Even when you’ve been diligent with tracking, it’s important to recognize when scalp irritation signals something more complex. Persistent inflammation, scabbing, or hair thinning could suggest an underlying dermatological condition such as seborrheic dermatitis, psoriasis, or even a fungal infection.⁵ These require medical treatment rather than product avoidance alone.
Seek a dermatologist if:
-
Symptoms persist for more than two weeks despite stopping new products.
-
You notice patches of hair loss or oozing.
-
Over-the-counter remedies cause worsening discomfort.
A dermatologist may recommend additional investigations such as fungal cultures, trichoscopy (scalp imaging), or biopsy if necessary. Addressing scalp inflammation early prevents long-term sensitivity and supports healthier hair growth.
At-Home Care Between Tests
While waiting for results or managing mild flare-ups, gentle home care can make a significant difference. Focus on maintaining scalp barrier integrity, which is the skin’s natural shield against allergens and irritants.
At-home tips:
-
Use fragrance-free, sulfate-free shampoos specifically labeled for sensitive or reactive scalps.
-
Avoid tight hairstyles or heavy oils that may trap heat and exacerbate irritation.
-
Apply cool compresses for temporary itch relief.
-
Use barrier-repair serums or masks containing ceramides, colloidal oatmeal, or zinc to calm inflammation.⁶
Always patch test new products behind the ear or on the inner arm for 48 hours before applying them to your scalp. Even hypoallergenic products can contain mild irritants for certain individuals.
If a flare-up occurs, note it in your trigger log and share the details with your dermatologist. This collaboration allows for continual refinement of your care routine.
How to Discuss Results with Your Dermatologist
Your patch test results are most powerful when combined with open, detailed discussion. Bring your trigger logs, photos, and a list of your regular products to every appointment. These records help your dermatologist design a care plan that feels personalized rather than restrictive.
Together, you might explore:
-
Ingredient substitutions: Safer alternatives that maintain desired effects without triggering reactions.
-
Routine simplification: Fewer products mean fewer potential irritants.
-
Barrier-repair strategies: Incorporating scalp treatments that rebuild lipid balance and moisture.
Your dermatologist may also suggest retesting after six to twelve months if your sensitivities evolve or if new ingredients enter your routine. A clear understanding of your skin’s behavior promotes confidence, helping you approach scalp care with knowledge and calm instead of fear or confusion.
Glossary
Allergen: A substance that can provoke an allergic reaction in sensitive individuals.
Patch Test: A diagnostic tool where allergens are applied to the skin to identify delayed allergic reactions.
Contact Dermatitis: Inflammation caused by direct contact with an irritant or allergen, leading to redness or itching.
Hypoallergenic: Formulated to minimize the risk of allergic reactions, though not completely allergen-free.
Methylisothiazolinone (MI): A preservative known to cause allergic contact dermatitis.
Seborrheic Dermatitis: A chronic skin condition causing flaking, itching, and redness, especially on the scalp.
Barrier Function: The skin’s ability to retain moisture and protect against irritants and pathogens.
Ceramides: Fatty molecules that help restore and maintain the skin barrier, reducing dryness and inflammation.
Trichoscopy: A non-invasive imaging technique used to examine scalp and hair disorders.
Claims Registry
| # | Claim | Source | Accessed | Anchor Extract | Notes |
|---|---|---|---|---|---|
| 1 | Patch testing identifies substances that trigger allergic reactions. | Lachapelle JM, et al. Contact Dermatitis, 2019. | 2025-10-26 (America/New_York) | "Patch testing remains the gold standard for diagnosing allergic contact dermatitis." | Peer-reviewed dermatology source. |
| 2 | Patch tests detect delayed hypersensitivity, not immediate reactions. | Zug KA, et al. Journal of the American Academy of Dermatology, 2020. | 2025-10-26 | "Patch testing identifies delayed type IV hypersensitivity responses." | Standard dermatologic reference. |
| 3 | Common allergens include PPD, fragrance mix, MI/MCI. | de Groot AC, Contact Dermatitis Monographs, 2021. | 2025-10-26 | "Fragrance mix and preservatives like MI are major sensitizers." | Reputable clinical compilation. |
| 4 | Results graded by reaction severity (redness, swelling, blistering). | European Society of Contact Dermatitis, Guidelines, 2018. | 2025-10-26 | "The grading system standardizes patch test results across clinics." | Official clinical guideline. |
| 5 | Persistent inflammation may indicate chronic conditions. | American Academy of Dermatology, 2023. | 2025-10-26 | "Chronic scalp inflammation warrants evaluation for psoriasis or seborrheic dermatitis." | Clinical practice guideline. |
| 6 | Ceramides support barrier repair. | Rawlings AV, International Journal of Cosmetic Science, 2022. | 2025-10-26 | "Topical ceramides enhance barrier recovery and reduce irritation." | Established cosmetic science research. |




