Patch Testing for Sensitive Scalps: Identifying Allergens Behind Irritation
Michele Marchand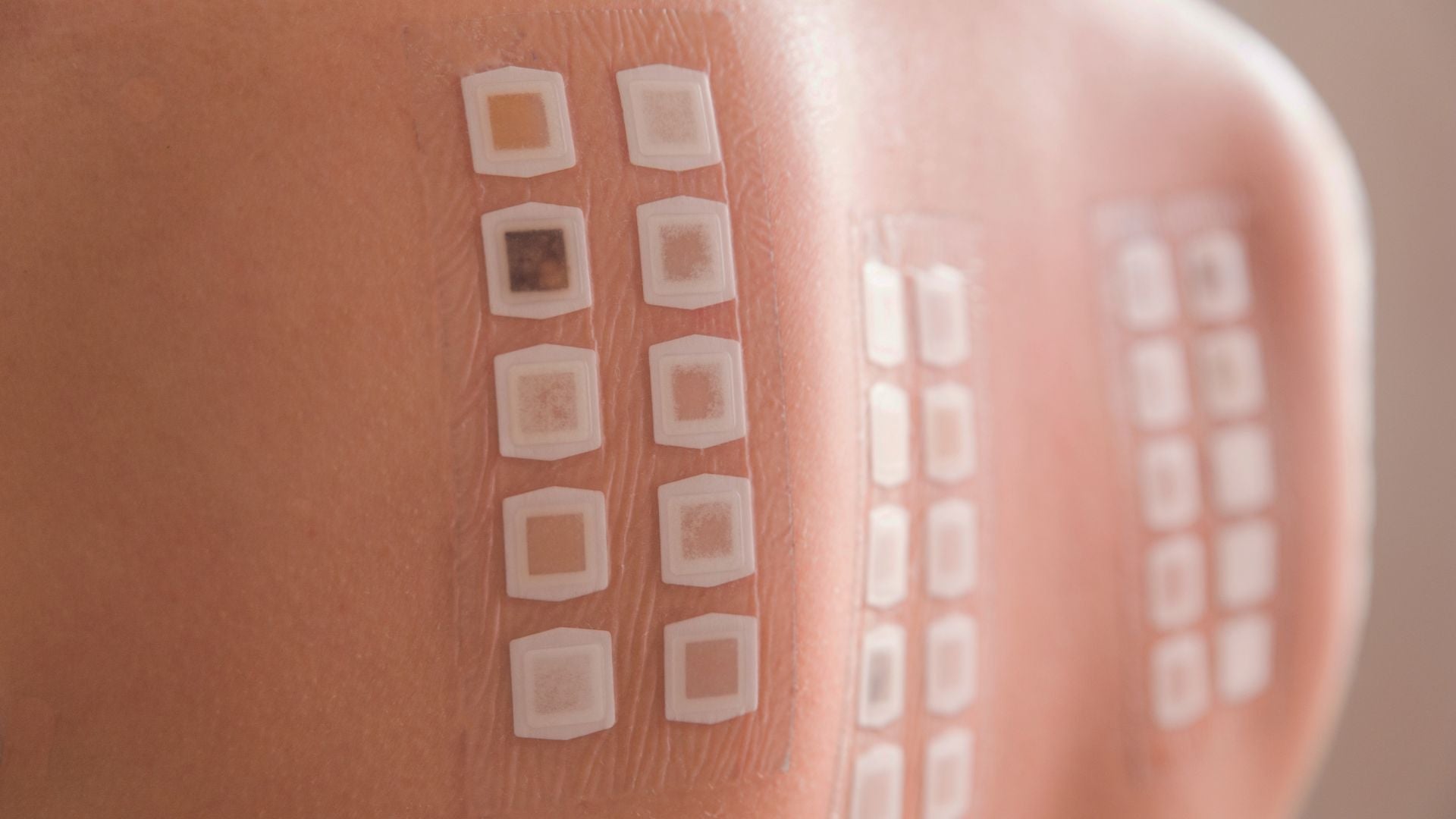
How does patch testing reveal the hidden causes of scalp irritation and allergies?
How Patch Testing Works: A Clear Guide for Sensitive Scalps
Subtitle: What happens during patch testing, and how can it uncover the cause of scalp irritation?
Table of Contents
- What is patch testing and why does it matter?
- How is a patch test performed step by step?
- What allergens are included in standard scalp panels?
- How are patch test results interpreted?
- How does patch testing help people with scalp conditions?
- What should you expect after a positive result?
- What are the limitations and risks of patch testing?
- How should you prepare for your patch test appointment?
- Final thoughts: taking control of scalp allergies
What is patch testing and why does it matter?
Patch testing is a diagnostic procedure used to identify allergic contact dermatitis, a condition where the skin develops inflammation after repeated exposure to an allergen. This differs from skin prick testing, which is used to evaluate immediate allergies such as pollen, dust mites, or foods that cause hives within minutes. Patch testing focuses on delayed immune responses that typically appear 48 to 96 hours after contact¹. For people struggling with scalp irritation, such as persistent redness, itching, burning, or flaking, patch testing can be a turning point in understanding what is happening beneath the surface.
Many individuals cycle endlessly through shampoos, conditioners, and hair treatments, hoping to stumble on a product that will not trigger discomfort. This trial-and-error approach is exhausting and often discouraging. Patch testing replaces guesswork with evidence. Instead of suspecting every new product, it isolates which ingredients or substances your immune system perceives as threats. With this clarity, patients can make informed decisions and avoid unnecessary frustration.
How is a patch test performed step by step?
The patch test protocol is standardized by dermatology societies around the world, ensuring the procedure is consistent, safe, and reliable. Although it requires multiple visits and a degree of patience, the payoff is clarity that lasts a lifetime. Here is what usually happens:
-
Preparation: During the first appointment, your dermatologist reviews your history of symptoms, personal care habits, and any medications you currently use. You may be asked to discontinue topical corticosteroids or strong skin creams a week before testing, since these can mask allergic reactions². In some cases, oral medications may also be reviewed.
-
Application: The test itself uses small chambers, tiny cups made of metal or plastic, filled with standardized allergen samples. These chambers are attached to adhesive strips and placed carefully on your back, since the area provides enough space for multiple test panels.
-
Waiting period: Once in place, the patches must remain undisturbed for 48 hours. During this time, patients are advised not to shower, swim, or engage in activities that cause heavy sweating, as moisture could dislodge the chambers.
-
First reading: After 48 hours, the patches are removed. The dermatologist examines your skin for any signs of redness or irritation. This early reading helps capture allergens that cause faster delayed reactions.
-
Second reading: A final evaluation is usually scheduled at 72 to 96 hours after application. This step is critical because some allergens produce very slow-onset reactions that would otherwise be missed if only an early reading were taken.
The procedure may feel inconvenient, but it is the only way to catch the immune system’s slow but significant responses. Many patients are surprised at which substances light up during testing, sometimes it is not the obvious shampoo or dye ingredient, but something subtle like a preservative or metal clasp.
What allergens are included in standard scalp panels?
Dermatologists rely on curated allergen panels designed to reflect the most common triggers for skin and scalp allergies. A baseline series is typically used for all patients and contains widely recognized irritants such as preservatives, fragrance mixes, and metals³. However, for patients with scalp-specific issues, additional focused allergens may be added.
Some of the most common scalp-related allergens include:
-
Hair dye chemicals: Paraphenylenediamine (PPD) is notorious for causing reactions, particularly in permanent hair dyes. Even low-level exposures may trigger strong scalp inflammation.
-
Fragrance mixes: Fragrance is one of the top causes of allergic contact dermatitis worldwide. Because shampoos, conditioners, and styling products often contain multiple fragrance compounds, mixtures are tested together.
-
Preservatives: Substances like methylisothiazolinone (MI), methylchloroisothiazolinone (MCI), and formaldehyde releasers are added to prevent bacterial growth in cosmetics but are frequent culprits for scalp allergies.
-
Nickel and metals: Hair accessories, clips, and even applicators for dyes or styling tools may contain nickel, which is one of the most common metal allergens.
-
Topical medications: Some treatments for scalp conditions, such as corticosteroid creams or minoxidil (commonly used for hair loss), can themselves provoke allergic reactions.
-
Botanical extracts: Natural-sounding ingredients like tea tree oil, lavender, or chamomile may seem gentle but are well-documented causes of contact allergies in sensitive individuals.
By tailoring the allergen panel to include both general and scalp-specific substances, dermatologists maximize the chances of identifying the true triggers.
How are patch test results interpreted?
Interpreting patch tests is a specialized skill that blends science with clinical judgment. After removal of the patches, the dermatologist looks closely for changes at each chamber site. Reactions are assessed for redness, swelling, infiltration, or small blisters, which indicate a true allergic reaction rather than simple irritation.
The International Contact Dermatitis Research Group (ICDRG) scoring system is widely used to standardize these observations. A “+” reaction indicates faint redness and infiltration, “++” suggests stronger inflammation with papules, and “+++” shows vesicles or blistering, which strongly confirms an allergy⁴. Negative reactions are marked with “–,” while doubtful results are noted as “?” if only minimal redness is present.
However, interpretation goes beyond the score. The dermatologist cross-references these results with your personal history. For example, a weak positive to a preservative may not matter if you never use products containing it. On the other hand, a strong positive to fragrance mix could directly explain years of unexplained scalp flares. Context is everything.
How does patch testing help people with scalp conditions?
For scalp conditions, patch testing is particularly valuable because symptoms often overlap with other disorders. Itching, redness, scaling, and flaking can appear in seborrheic dermatitis, psoriasis, and eczema, making it difficult to distinguish allergic contact dermatitis without testing. Many individuals misinterpret their scalp symptoms as “just dandruff,” while in reality, the immune system is reacting to a product ingredient.
By confirming or ruling out allergic contact dermatitis, patch testing allows for more precise treatment. If an allergen is identified, management shifts from endless experimentation to targeted avoidance. Patients no longer need to avoid all hair products; instead, they can confidently use safe options while steering clear of specific triggers. This reduces frustration and often leads to dramatic improvements in quality of life.
What should you expect after a positive result?
Discovering an allergen during patch testing provides a roadmap for recovery. The next steps involve strict but manageable avoidance of the identified substance. Dermatologists typically provide detailed ingredient lists and may recommend databases or smartphone apps that help patients cross-check products.
Practical recommendations include:
-
Check labels thoroughly: Learn to spot both the chemical name and its common synonyms.
-
Switch to fragrance-free or hypoallergenic products: These are less likely to contain hidden triggers.
-
Keep a product diary: Note any changes in symptoms when starting a new shampoo, conditioner, or scalp treatment.
-
Consider alternative treatments: For hair dye allergies, options like henna or PPD-free dyes may be viable.
-
Inform your stylist or barber: This prevents accidental exposure during professional treatments.
In most cases, patients who successfully avoid the allergen experience significant improvements within weeks to months. While it requires vigilance, the effort pays off with long-term scalp comfort.
What are the limitations and risks of patch testing?
Patch testing is highly effective but not flawless. Patients should be aware of its limitations:
-
False positives: Sometimes the skin reacts mildly to an allergen, but the response has no real-world significance.
-
False negatives: Certain uncommon allergens may not be included in the panels, leading to missed diagnoses.
-
Skin irritation: Rarely, the adhesive or chambers themselves may cause temporary irritation.
-
Time and lifestyle disruption: Because the patches must remain in place for two days and follow-up visits are required, some patients find the process inconvenient.
Despite these challenges, patch testing is widely regarded as the gold standard for diagnosing allergic contact dermatitis⁵. Few other methods can provide the same level of clarity and long-term benefit.
How should you prepare for your patch test appointment?
Good preparation can maximize the accuracy of patch test results and minimize discomfort. Before the test:
-
Stop topical corticosteroids or immunosuppressive creams on the back at least a week before, unless your doctor gives other instructions.
-
Bring your personal care products, shampoos, conditioners, styling gels, or treatments, so the dermatologist can evaluate ingredients directly or test specific substances.
-
Wear loose, comfortable clothing that will not rub against or dislodge the patches.
-
Plan your schedule to accommodate the 48-hour waiting period and at least two clinic visits.
-
Avoid tanning or sunburn on your back in the days leading up to the test, as damaged skin can interfere with accurate results.
With proper preparation, the test provides the clearest possible picture of your unique skin sensitivities.
Final thoughts: taking control of scalp allergies
Living with a sensitive scalp can be exhausting. The uncertainty about which product will cause a reaction often leads to frustration, embarrassment, and even avoidance of normal grooming routines. Patch testing offers a path out of that cycle. By uncovering specific allergens, it transforms vague discomfort into a clear diagnosis and manageable treatment plan.
For most patients, the relief comes not only from improved symptoms but also from the reassurance of having concrete answers. With professional support and practical avoidance strategies, the scalp can recover, and confidence can return. If you have struggled with unexplained irritation, patch testing is worth discussing with a dermatologist. The journey toward relief often begins with the simple act of identifying what your skin is trying to tell you.
Glossary
-
Allergic contact dermatitis: A skin reaction caused by immune sensitivity to substances touching the skin.
-
Patch testing: A method for identifying delayed-type skin allergies by applying allergens under patches.
-
Allergen panel: A curated group of common allergy-causing substances used in testing.
-
Paraphenylenediamine (PPD): A chemical in permanent hair dyes, often linked to allergic reactions.
-
Preservatives: Chemicals that prevent microbial growth in cosmetics, sometimes triggering allergies.
-
Fragrance mix: A blend of common perfume chemicals tested together in patch panels.
-
Nickel: A metal frequently causing allergic reactions, found in jewelry and hair tools.
-
Seborrheic dermatitis: A chronic scalp condition causing redness, itching, and flaking, unrelated to allergies.
-
Psoriasis: An autoimmune skin condition with thick, scaly patches.
-
Topical corticosteroids: Anti-inflammatory creams applied to the skin, which may interfere with patch test results.
Claims Registry
| Citation # | Claim(s) Supported | Source Title + Authors + Year + Venue | Anchor Extract | Notes |
|---|---|---|---|---|
| 1 | Patch testing identifies delayed allergic reactions, unlike skin prick tests. | "Patch Testing in Contact Dermatitis" – Lachapelle JM, Maibach HI, 2012, Springer | "Patch testing detects delayed hypersensitivity reactions occurring 48–96 hours after exposure." | Foundational dermatology reference. |
| 2 | Patients may be asked to stop steroids before patch testing. | American Academy of Dermatology, Patch Testing Guidelines, 2022 | "Topical corticosteroids may suppress reactions and should be discontinued prior to testing." | Clinical guideline. |
| 3 | Allergen panels include preservatives, fragrances, dyes, and metals. | European Society of Contact Dermatitis, Standard Series Update, 2020 | "The baseline series covers preservatives, fragrances, hair dye chemicals, and metals." | European consensus guideline. |
| 4 | Patch test results are graded using international scoring system. | International Contact Dermatitis Research Group Criteria, 2019 | "+ denotes erythema, ++ infiltration, +++ vesicles." | Standard scoring system. |
| 5 | Patch testing is the gold standard for allergic contact dermatitis diagnosis. | "Contact Dermatitis" – Johansen JD et al., 2015, New England Journal of Medicine | "Patch testing remains the gold standard for diagnosing allergic contact dermatitis." | High-impact medical review. |




