Desensitization and Barrier Reset: Stepwise Protocol
Michele Marchand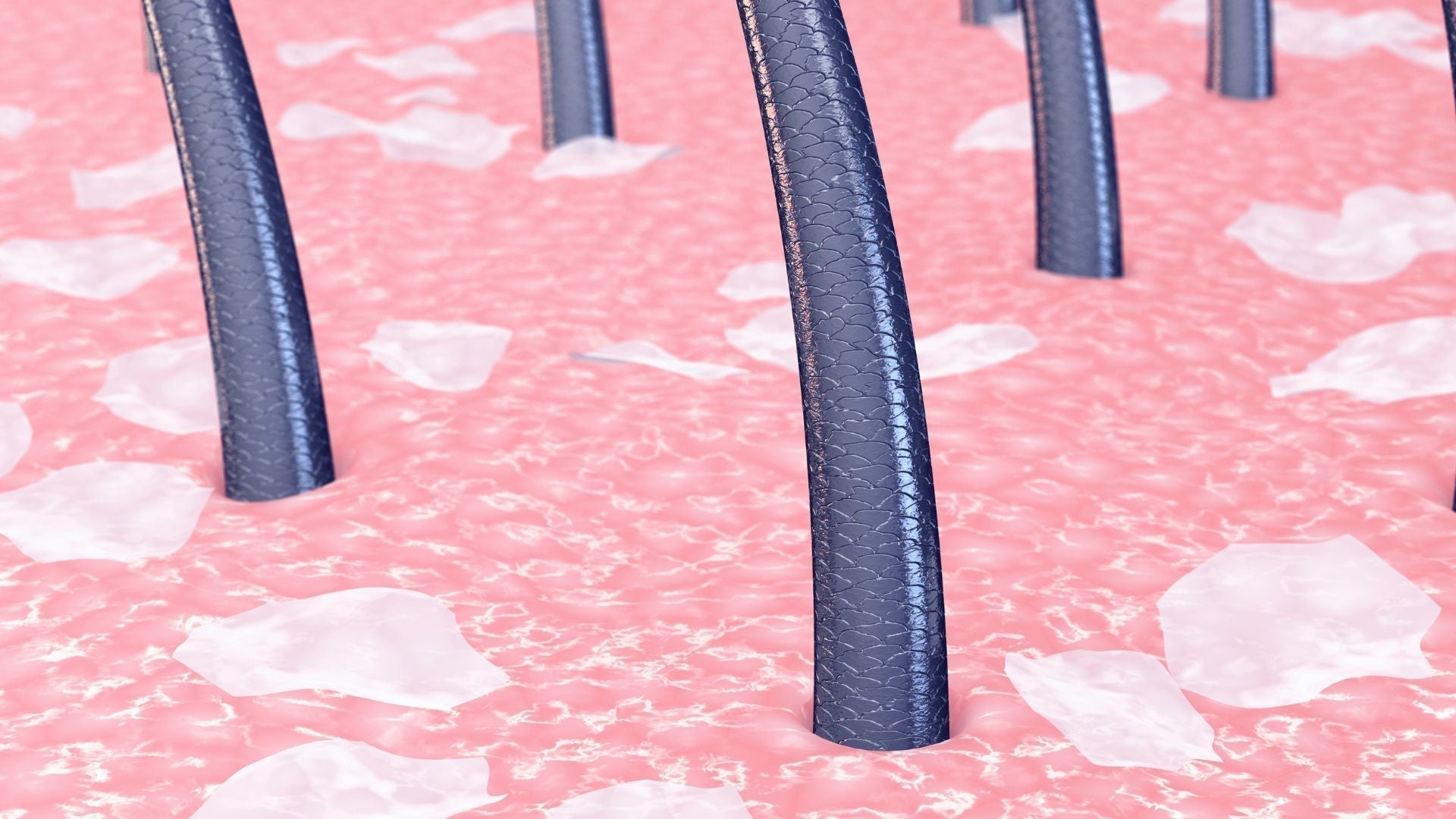
Table of Contents
- Why do sensitive scalps need a structured reset?
- What exactly is desensitization in scalp care?
- Step 1: Eliminate irritants without stripping the scalp
- Step 2: Introduce hydration gradually
- Step 3: Restore the barrier with targeted lipids
- Step 4: Soothe nerve endings with anti-inflammatory agents
- Step 5: Build resilience with controlled exposure
- Step 6: Maintain with consistent routines
- When should you see a dermatologist?
- Gentle daily practices that reinforce the protocol
- The takeaway: patience and persistence pay off
- Glossary
- Claims Registry
Why do sensitive scalps need a structured reset?
A sensitive scalp is more than just an occasional tingle or itch. It reflects a disrupted skin barrier, which is the scalp’s natural defense against irritants, microbes, and moisture loss. When this barrier becomes compromised, everyday triggers like shampoo, temperature shifts, or even stress can feel overwhelming. Studies estimate that between 44% and 52% of adults experience sensitive scalp symptoms¹. This means nearly half the population may be struggling with discomfort that is often dismissed or misunderstood. Understanding that sensitivity is a biological signal, not a personal failing, is the first step toward effective care.
A stepwise desensitization and barrier reset protocol aims to reduce reactivity by calming nerve endings, lowering inflammation, and restoring barrier lipids. Unlike quick-fix treatments that promise overnight relief, this approach acknowledges that healing requires time. The key is pacing: introducing supportive steps gradually so the scalp learns to tolerate more over time. Just as physical therapy retrains muscles after an injury, desensitization retrains the scalp’s nervous system to stop overreacting to minor triggers. Over time, this structured care can bring lasting comfort instead of temporary relief.
What exactly is desensitization in scalp care?
Desensitization means lowering the scalp’s exaggerated response to normal stimuli. In dermatology, it often involves repeated, controlled exposure to gentle interventions that retrain sensory nerve endings. Think of it as teaching the scalp to “unlearn” its over-sensitivity. On the scalp, this can include fragrance-free cleansing, hydration, and barrier-restoring agents such as ceramides (natural lipids that repair the skin’s barrier). The process is not about toughening up the skin but about helping it return to baseline balance.
Barrier reset complements desensitization. A barrier reset protocol focuses on repairing the outermost layer of the scalp skin, the stratum corneum, so it can once again act as a shield. When the barrier is intact, it prevents irritants from penetrating and reduces water loss. Together, desensitization and barrier repair reduce stinging, itching, and burning sensations, giving the scalp a chance to function normally again. Patients often notice not only physical comfort but also emotional relief, since constant irritation can affect mood, sleep, and overall quality of life.
Step 1: Eliminate irritants without stripping the scalp
The first action is subtraction. Remove unnecessary triggers such as sulfated shampoos, high-alcohol styling products, or frequent heat exposure. Instead, use a mild, sulfate-free cleanser. Ingredients like glycerin and aloe vera can hydrate while cleansing, creating a base of comfort instead of stripping away natural oils. Avoid fragrance, which is a common cause of contact sensitivity². This subtraction phase often takes two to three weeks, during which the scalp can begin to calm down and reestablish a healthier baseline.
For many, this stage feels like a detox. Irritation often improves noticeably once hidden triggers are removed. It is tempting to immediately add soothing oils or treatments, but patience is crucial. The scalp needs space to “quiet down” before introducing new variables. Think of this step as laying the foundation of a house: everything that follows will be stronger if the base is stable.
Tip: Wash less frequently at first, every 2–3 days instead of daily, to avoid repeated disruption of the barrier. If sweating or styling demands more frequent cleansing, choose a micellar water-based scalp rinse between washes.
Step 2: Introduce hydration gradually
Once triggers are removed, controlled hydration helps reduce tightness and restore comfort. The scalp, like the skin on the face, requires both water and oil to stay balanced. Use lightweight, fragrance-free scalp tonics or sprays containing humectants (water-attracting molecules) like hyaluronic acid. These ingredients pull water into the outer layer of the scalp, reducing the sensation of dryness.
The key here is gradual introduction. Apply sparingly at first to a small section of the scalp. If no burning or stinging occurs after 48 hours, expand to the whole scalp. This patch-testing approach prevents flare-ups and builds trust in the product. Some patients may benefit from layering hydration with a light occlusive, such as squalane, which locks in moisture without clogging follicles. Over time, consistent hydration not only improves comfort but also enhances elasticity, reducing the likelihood of micro-irritations.
Tip: Hydrate when the scalp is still slightly damp from washing, which enhances absorption and comfort.
Step 3: Restore the barrier with targeted lipids
Barrier restoration requires replenishing missing lipids. Look for leave-on products with ceramides, cholesterol, and fatty acids. These mimic the scalp’s own protective layer. Clinical trials show that ceramide-containing creams significantly improve barrier integrity in sensitive skin³. Applied once daily for several weeks, these lipids reduce reactivity, scaling, and dryness.
Think of barrier lipids as the mortar between the bricks of a wall. Without them, the barrier leaks, leaving the scalp vulnerable. Replacing those lipids not only strengthens protection but also reduces the nerve hyper-reactivity that drives sensitivity. Patients who stick with lipid repair often report less tightness and an improved tolerance to products they once had to avoid.
Tip: Night application allows lipids to absorb while the scalp is less exposed to external stressors such as sun, wind, or pollution.
Step 4: Soothe nerve endings with anti-inflammatory agents
Sensitive scalps often involve hyperactive sensory nerves, which misinterpret mild sensations as pain or burning. Calming these nerves requires both anti-inflammatory support and gentle persistence. Botanical agents like panthenol (pro-vitamin B5) have natural soothing properties. They reduce redness and deliver hydration simultaneously.
In medical settings, dermatologists may recommend mild corticosteroid solutions for acute flares, but these should be short-term and physician-guided. Niacinamide, a form of vitamin B3, has been shown to reduce inflammation while strengthening the barrier⁴. By increasing the production of ceramides, niacinamide works at the intersection of barrier repair and nerve calming. Introducing these agents slowly ensures tolerance while building long-term resilience.
Tip: Apply anti-inflammatory leave-on products during times of stress, such as seasonal changes or after coloring treatments, when the scalp is more reactive.
Step 5: Build resilience with controlled exposure
As comfort increases, resilience-building becomes important. Controlled exposure means gradually reintroducing once-problematic but necessary elements, such as slightly stronger cleansers, hair dye, or increased wash frequency. This helps train the scalp to tolerate normal life again. Just as allergy therapies work through slow exposure to allergens, scalp desensitization requires calculated reintroduction.
The goal is not perfection but tolerance. A completely sensitivity-free scalp may not be realistic, but reducing the intensity and frequency of symptoms is. Patients often find that, with resilience training, their scalp no longer reacts to mild weather changes, occasional product swaps, or gentle styling practices. This stage is empowering, as it shifts the focus from avoidance to confidence.
Tip: Keep a symptom diary when reintroducing potential irritants. Note what was added, how quickly, and any sensations felt. This creates a personalized map of tolerance.
Step 6: Maintain with consistent routines
Once stability is achieved, consistency matters more than novelty. Stick with products that have proven tolerable. Avoid hopping between brands in search of something “better.” A stable routine maintains results and prevents regression. Dermatologists often remind patients that sensitive skin thrives on predictability, not experimentation.
Maintenance also includes lifestyle habits: gentle cleansing, adequate hydration, stress management, and sun protection. Think of these as the four pillars of scalp stability. Missing one may not cause immediate chaos, but over time, the cracks can show. Checking in with a dermatologist once or twice a year for reassurance and routine adjustment can help keep progress on track.
Tip: Refresh your routine seasonally. Winter dryness or summer humidity may call for small adjustments, but keep the core products consistent.
When should you see a dermatologist?
If scalp sensitivity persists despite careful routines, or if symptoms escalate to hair shedding, bleeding, or infection, professional evaluation is essential. Conditions such as seborrheic dermatitis, psoriasis, or allergic contact dermatitis may mimic general sensitivity but require specific treatments. A dermatologist can perform patch testing to identify hidden allergens and prescribe advanced therapies such as calcineurin inhibitors or specialized shampoos.
Ignoring persistent sensitivity risks worsening symptoms and unnecessary suffering. A tailored plan from a dermatologist can uncover hidden triggers, guide product selection, and offer relief much faster than trial and error alone. Even one consultation can clarify months of confusion.
Gentle daily practices that reinforce the protocol
-
Use lukewarm water instead of hot when washing, as heat worsens barrier disruption.
-
Choose wide-toothed combs to minimize mechanical irritation and reduce hair breakage.
-
Protect the scalp from direct sun exposure with hats or mineral sunscreens, since UV radiation worsens inflammation.
-
Manage stress through sleep, exercise, and mindfulness, as stress can amplify nerve sensitivity.
-
Limit tight hairstyles, which can place unnecessary tension on the scalp.
-
Keep a balanced diet rich in omega-3 fatty acids, zinc, and antioxidants, which support skin health from within.
-
Maintain indoor humidity during winter months to reduce dryness that worsens sensitivity.
The takeaway: patience and persistence pay off
Sensitive scalp care is not a sprint but a measured reset. By eliminating irritants, rehydrating gradually, restoring lipids, and calming nerve activity, the scalp can regain its natural balance. The protocol is stepwise because healing requires patience, not overload. Each small change builds toward resilience. With consistency, most people can dramatically reduce their discomfort and live with a healthier, calmer scalp.
Most importantly, remember that sensitivity is not a personal weakness. It is a signal from the body, asking for care and protection. Listening to that signal and responding with structured support makes all the difference. A calmer scalp often brings more than physical relief: it restores confidence, improves quality of life, and allows individuals to focus on what truly matters instead of constant discomfort.
Glossary
-
Barrier reset: A skincare approach that restores the protective outer layer of skin.
-
Ceramides: Lipid molecules that strengthen and repair the skin barrier.
-
Desensitization: Reducing exaggerated nerve responses to normal stimuli.
-
Humectants: Ingredients that attract water to the skin, such as glycerin or hyaluronic acid.
-
Niacinamide: A form of vitamin B3 with anti-inflammatory and barrier-strengthening properties.
-
Seborrheic dermatitis: A scalp condition with flaking, redness, and irritation.
-
Stratum corneum: The outermost layer of skin that serves as a protective barrier.
-
Bisabolol: A calming compound derived from chamomile with anti-inflammatory effects.
-
Panthenol: Also known as pro-vitamin B5, helps hydrate and soothe the scalp.
-
Occlusives: Ingredients that form a protective film to prevent water loss, such as squalane or petrolatum.
Claims Registry
| Citation # | Claim(s) supported | Source title + authors + year + venue | Anchor extract | Notes |
|---|---|---|---|---|
| 1 | 44–52% of adults experience sensitive scalp symptoms | Misery L et al., "Sensitive scalp: does this condition exist?" 2008, Br J Dermatol | "Sensitive scalp was reported by 44.2% of women and 32.0% of men." | Peer-reviewed study establishing prevalence. |
| 2 | Fragrance is a common cause of contact sensitivity | Zug KA et al., "Patch-testing North American dermatitis patients" 2009, Dermatitis | "Fragrance mix was the most common allergen detected." | Widely cited contact allergy study. |
| 3 | Ceramide-containing creams improve barrier integrity | Kelleher MM et al., "Barrier enhancement for eczema prevention" 2015, J Allergy Clin Immunol | "Topical application of ceramides enhances barrier function." | Clinical data on ceramides. |
| 4 | Niacinamide reduces inflammation and strengthens barrier | Gehring W., "Nicotineamide in dermatology" 2004, J Cosmet Dermatol | "Topical nicotinamide increases ceramide synthesis, improves barrier function, and exerts anti-inflammatory effects." | Key review on niacinamide benefits. |




