Follicular Occlusion and Fibrosis: How Blocked Follicles Lead to Scarring
Michele Marchand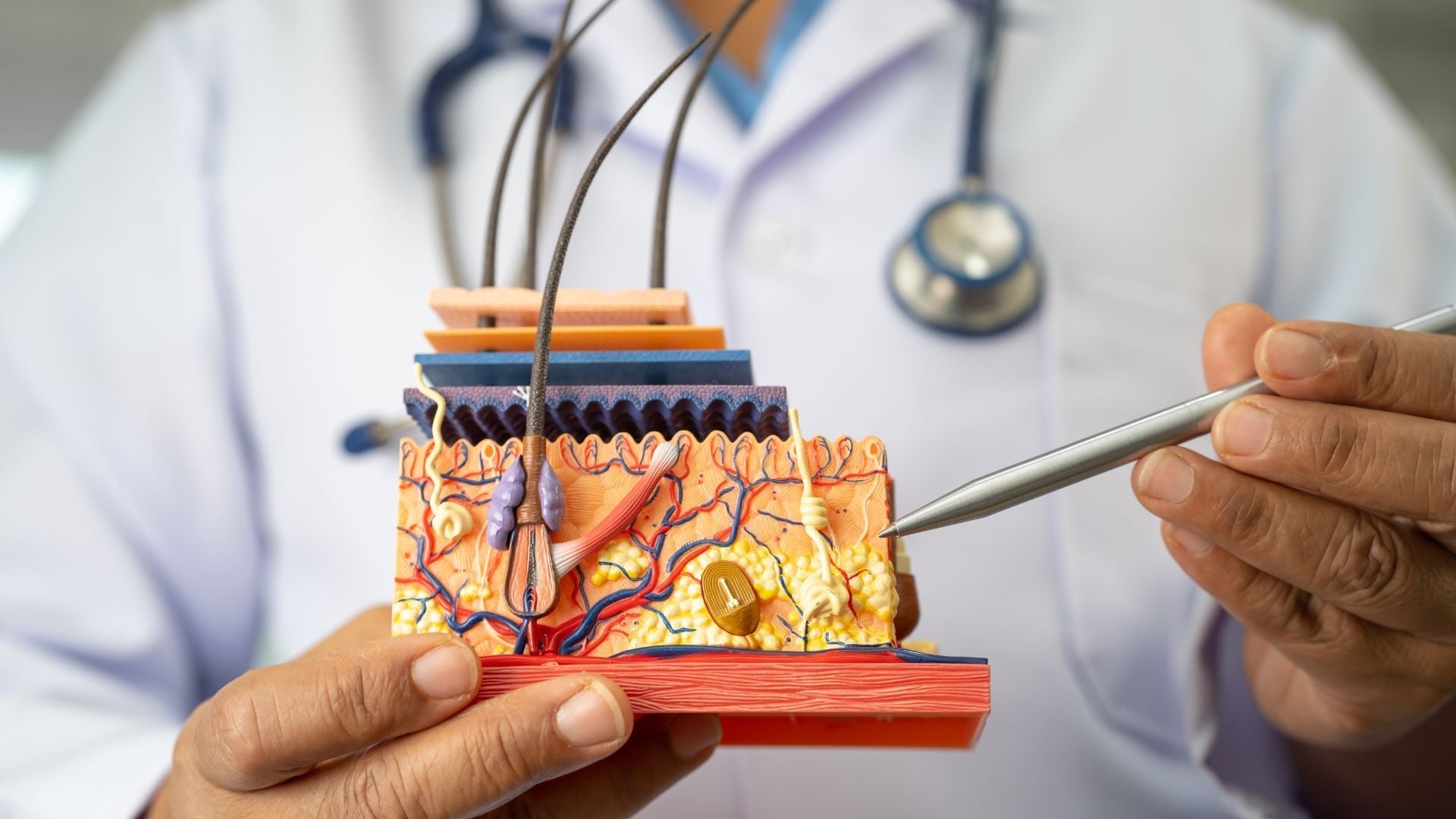
What causes blocked hair follicles to scar, and how can early scalp care help?
Table of Contents
- What is follicular occlusion and why does it matter?
- How does occlusion begin in the scalp?
- What is fibrosis and how does it affect the scalp?
- How do occlusion and fibrosis connect?
- Which scalp conditions are linked to follicular occlusion?
- What can increase your risk of follicular occlusion?
- How do dermatologists diagnose fibrosis in the scalp?
- What treatments can help with follicular occlusion?
- What can you do at home to protect your scalp?
- When should you see a dermatologist?
- Key takeaway
What is follicular occlusion and why does it matter?
Follicular occlusion occurs when the small opening of a hair follicle becomes blocked. Hair follicles are tiny but essential structures in the skin that produce each strand of hair. They need an open pathway to release sebum (the natural oil produced by the scalp), shed old skin cells, and allow the hair shaft to emerge. When this pathway is obstructed by oil, dead skin cells, or external debris, the follicle becomes stressed.
A blocked follicle can trap bacteria, increase local inflammation, and disrupt the delicate balance of the scalp environment. This disruption can create redness, itching, and bumps, and in some cases, it triggers long-term inflammatory cycles. If these cycles continue, the body may respond by building scar tissue around the follicle. This scarring, known as fibrosis, gradually destroys the follicle’s ability to produce hair. Unlike temporary hair shedding, scarring hair loss caused by fibrosis is permanent. This is why understanding follicular occlusion is crucial for anyone who experiences recurrent scalp irritation or unexplained thinning.
How does occlusion begin in the scalp?
Follicular occlusion usually develops slowly and often goes unnoticed until symptoms appear. The process begins with a buildup at the follicle entrance. Several overlapping factors can cause this blockage:
-
Sebum overproduction: Sebaceous glands, which sit alongside the follicle, sometimes produce more oil than the scalp can handle. Hormonal changes during puberty, pregnancy, or menopause can heighten this activity. Medications such as anabolic steroids or testosterone therapy can also stimulate oil glands.
-
Keratin buildup: Keratin is the structural protein that forms hair and skin. Normally, dead keratinocytes (skin cells) shed smoothly. But when shedding slows, they clump together with sebum and form plugs.
-
Microbial imbalance: The scalp hosts a community of bacteria and yeast that usually coexist in balance. When certain microbes overgrow, they provoke inflammation and worsen blockage.
-
External irritants: Products that are heavy, oily, or difficult to wash out can sit on the scalp and mix with natural oils. Pollution and dust particles can also add to buildup.
For individuals with sensitive scalps, these triggers often reinforce one another. An increase in sebum thickens keratin plugs, while microbial changes inflame the follicle. The result is a repeating cycle of congestion and irritation.
What is fibrosis and how does it affect the scalp?
Fibrosis is the medical term for scarring inside tissue. It represents the body’s natural attempt to heal after injury, but on the scalp, this repair process can be destructive. When a follicle experiences frequent inflammation, the immune system sends in cells that stimulate the production of collagen. Collagen is a protein that provides strength and structure to the skin. In moderation, it helps close wounds. In excess, it creates stiff scar tissue.
Inside the scalp, fibrosis thickens the tissue surrounding follicles. This scar tissue restricts blood flow, reduces oxygen delivery, and compresses the delicate environment where the follicle normally thrives. As the area becomes rigid, hair shafts grow thinner and eventually stop emerging. In advanced stages, follicles can disappear completely, leaving behind shiny, smooth patches where hair once grew.
The key problem with fibrosis is its permanence. Unlike mild inflammation, which can subside once the trigger is removed, scar tissue cannot be reversed easily. This makes early recognition and intervention essential.
How do occlusion and fibrosis connect?
Follicular occlusion and fibrosis are not separate problems, they are two stages of the same damaging cycle. When the follicle becomes blocked, inflammation is almost inevitable. This inflammation may flare up, calm down, and then flare again when the blockage repeats. With each round, the immune system lays down more collagen. Over time, the follicle becomes trapped in an environment it cannot survive in.
This progression explains why scalp care is not just about comfort but also about prevention. Early symptoms like tenderness, itching, or small bumps are not merely cosmetic nuisances. They are warning signals. If ignored, they may set off the pathway toward fibrosis and irreversible hair loss. Addressing follicular occlusion in its earliest stages can protect scalp health for the long term.
Which scalp conditions are linked to follicular occlusion?
Several well-known dermatological disorders fall under what doctors call the “follicular occlusion spectrum.” These include:
-
Acne keloidalis nuchae: Small, firm bumps at the back of the neck that can merge into larger scars. Often seen in individuals who shave or have tightly curled hair.
-
Folliculitis decalvans: A chronic scalp condition where follicles become inflamed, leading to scarring and progressive hair loss. It is one of the most common causes of permanent scarring alopecia.
-
Dissecting cellulitis of the scalp: Painful nodules that may connect under the skin, leak pus, and form large scarred patches.
-
Hidradenitis suppurativa: A systemic condition marked by painful boils, most often in body folds, but sharing the same follicular occlusion pathway.
Not all cases of follicular occlusion progress to these conditions, but their shared pathway highlights the importance of early prevention. Recognizing the early warning signs may reduce the risk of developing chronic, scarring disorders.
What can increase your risk of follicular occlusion?
Certain factors make individuals more likely to develop follicular occlusion and subsequent fibrosis:
-
Genetics: A family history of scarring scalp disorders raises personal risk.
-
Hormonal shifts: Higher androgen levels stimulate oil production, creating an environment ripe for blockage.
-
Skin type: People with oily scalps or dense hair may trap sweat and debris more easily.
-
Hair care habits: Heavy oils, waxes, or styling products that coat the scalp can block follicles. Infrequent washing or poor rinsing may worsen the problem.
-
Lifestyle influences: Chronic stress, inadequate sleep, and diets high in refined sugars can raise systemic inflammation, making flare-ups more intense.
-
Mechanical irritation: Tight hairstyles, frequent helmet use, or friction from headgear can inflame follicles.
Awareness of these risk factors empowers individuals to adjust habits and reduce stress on their follicles before permanent changes occur.
How do dermatologists diagnose fibrosis in the scalp?
Diagnosis begins with a careful clinical examination. A dermatologist will observe the scalp for redness, swelling, or shiny patches where follicles appear absent. They may gently press or palpate the area to detect tenderness.
Two diagnostic tools are commonly used:
-
Trichoscopy: A magnified scalp imaging technique that allows dermatologists to see follicle openings, scaling, and vascular changes. It is noninvasive and highly informative.
-
Scalp biopsy: A small sample of scalp tissue taken under local anesthesia. This test confirms whether fibrosis has developed and helps distinguish between temporary follicular occlusion and true scarring alopecia.
By combining history, visual inspection, and targeted testing, dermatologists can provide clarity and guide treatment decisions.
What treatments can help with follicular occlusion?
Treatment options depend on whether the problem is at the stage of occlusion, inflammation, or fibrosis.
For early occlusion (before scarring):
-
Shampoos containing salicylic acid or zinc pyrithione to gently exfoliate and reduce microbial buildup.
-
Antimicrobial washes to rebalance bacteria and yeast.
-
Topical anti-inflammatory treatments, such as mild corticosteroid lotions, to calm irritation.
For active inflammation:
-
Prescription antibiotics (oral or topical) to target bacterial overgrowth.
-
Intralesional corticosteroid injections directly into inflamed areas to reduce immune activity.
-
Light-based therapies like photodynamic therapy in select cases.
For established fibrosis:
-
Anti-fibrotic medications are still being studied, but early research is promising.
-
Regenerative techniques such as platelet-rich plasma (PRP) or microneedling may improve blood supply and slow progression.
-
Hair transplantation may be possible if enough healthy scalp remains, though success depends on the degree of scarring.
What can you do at home to protect your scalp?
Medical treatment is essential, but daily habits influence scalp health as well. Supportive steps include:
-
Washing regularly with a gentle, fragrance-free shampoo to reduce buildup without stripping the scalp.
-
Avoiding heavy oils or thick styling products that may block follicles.
-
Using lukewarm water instead of very hot water, which can worsen inflammation.
-
Managing stress with mindfulness, physical activity, or relaxation techniques, since stress hormones can worsen scalp inflammation.
-
Keeping a scalp diary to track flare-ups, noting diet, stress, products used, and environmental changes. This helps dermatologists identify patterns.
Tip: Early action matters. If irritation, tenderness, or small bumps persist despite good hygiene, consider it a sign to seek medical advice.
When should you see a dermatologist?
Some scalp concerns improve with gentle care, but certain warning signs mean professional evaluation is necessary. Seek help if:
-
Patches of hair loss are accompanied by redness or shiny scarring.
-
Recurrent folliculitis fails to respond to mild shampoos or topical remedies.
-
Painful nodules, draining bumps, or spreading inflammation appear.
Dermatologists can distinguish temporary problems from serious scarring conditions. Timely diagnosis not only improves comfort but also preserves follicles that might otherwise be lost permanently.
Key takeaway
Follicular occlusion and fibrosis are interconnected stages of scalp damage. What begins as a simple blockage can escalate into inflammation and eventually scarring. The result is permanent follicle loss and irreversible hair thinning. By paying attention to early signs and seeking treatment, individuals can protect their scalp health and preserve hair growth.
Glossary
-
Follicle: The tiny skin structure from which hair grows.
-
Occlusion: Blockage of the follicle opening.
-
Sebum: Natural oil produced by sebaceous glands.
-
Keratin: Protein that makes up skin and hair; excessive buildup can block follicles.
-
Fibrosis: Formation of scar tissue that stiffens and thickens skin.
-
Collagen: Protein that provides structure in skin and scar tissue.
-
Inflammation: Body’s immune response to irritation or infection.
-
Folliculitis: Inflammation of one or more hair follicles.
-
Trichoscopy: Magnified scalp imaging used in dermatology.
-
PRP (Platelet-Rich Plasma): A treatment that uses a patient’s own blood components to support healing.
Claims Registry
| Citation # | Claim(s) Supported | Source | Anchor Extract | Notes |
|---|---|---|---|---|
| 1 | Repeated inflammation can lead to fibrosis and permanent hair loss | Olsen EA, “Scarring alopecia: clinical and pathophysiology review,” J Am Acad Dermatol, 2005 | “Repeated follicular inflammation induces fibrosis and permanent follicular damage.” | Authoritative dermatology review. |
| 2 | Disorders like folliculitis decalvans and dissecting cellulitis involve follicular occlusion | Powell JJ, et al., “Follicular occlusion syndromes,” Clin Exp Dermatol, 2009 | “Acne conglobata, hidradenitis suppurativa, and folliculitis decalvans are unified by follicular occlusion.” | Clinical overview of related syndromes. |
| 3 | Corticosteroid injections reduce inflammation in scarring alopecias | Kang H, et al., “Treatment of primary cicatricial alopecias,” Dermatol Ther, 2008 | “Intralesional corticosteroids are first-line therapy for active inflammation.” | Evidence-based treatment guideline. |
| 4 | PRP and microneedling show potential benefit in early fibrosis | Gentile P, et al., “Scalp fibrosis and regenerative approaches,” Stem Cells Int, 2019 | “PRP and microneedling may improve vascularity in early fibrosis.” | Peer-reviewed regenerative medicine article. |
| 5 | Stress, sleep, and diet influence scalp inflammation | Arck PC, et al., “Stress and the hair follicle,” Exp Dermatol, 2011 | “Stress-induced signals impair follicle immune privilege and promote inflammation.” | Well-cited paper linking lifestyle and scalp health. |




