How Inflammatory Scalp Pathways Work
Michele Marchand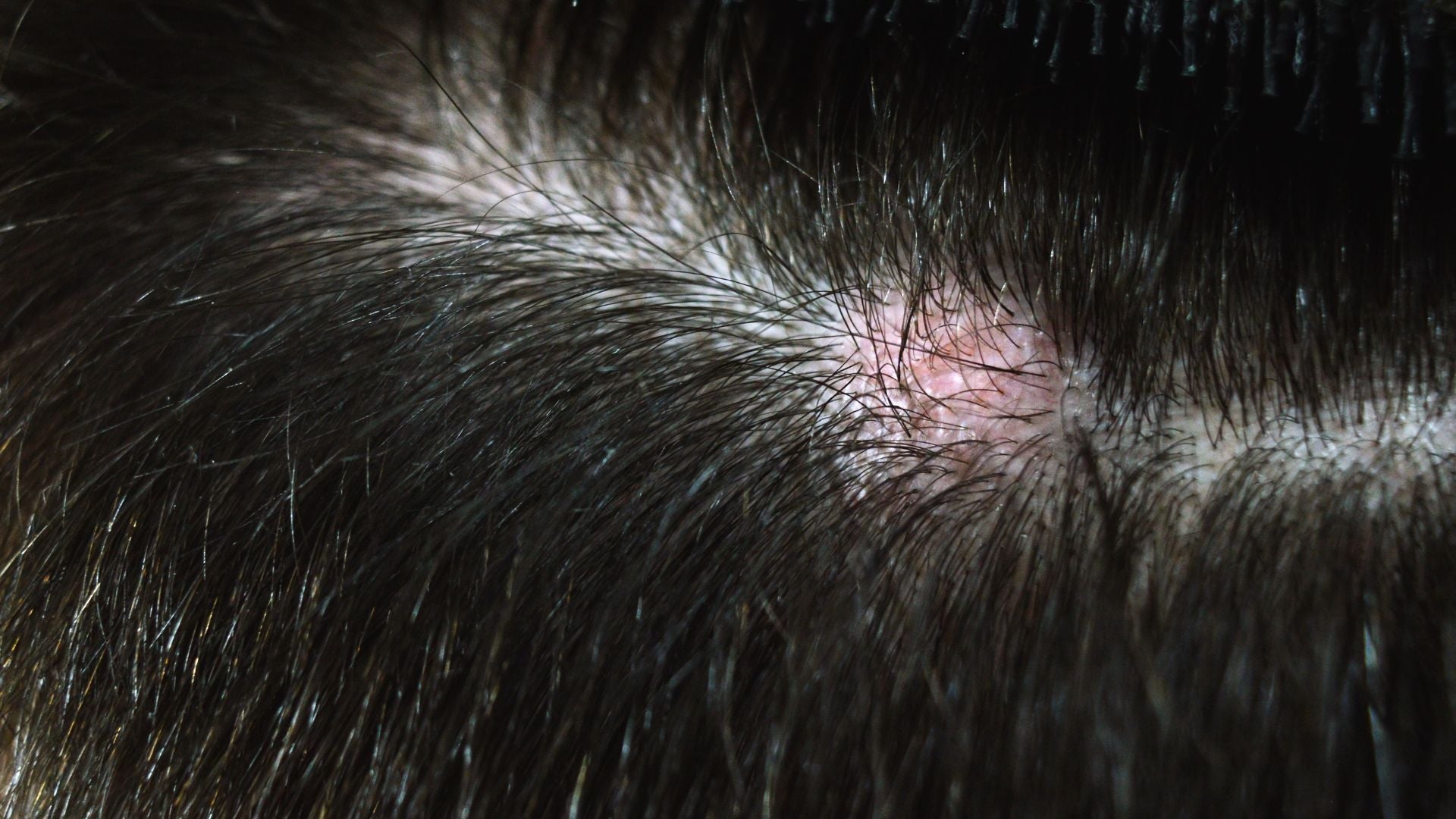
What happens when cytokines and immune responses trigger scalp irritation?
Table of Contents
- Why inflammation shows up on the scalp
- What are cytokines and why do they matter on the scalp?
- How local immune activation works in the scalp
- Which pathways are most important in scalp inflammation?
- How does this connect to scalp conditions you may know?
- What treatments target inflammatory pathways?
- When should you see a dermatologist?
- Key takeaways for sensitive scalps
Why inflammation shows up on the scalp
Your scalp is one of the most active pieces of real estate on your body. It is covered with thousands of hair follicles, oil glands, and tiny blood vessels that keep hair and skin alive. Because it is so active, it is also one of the places most likely to show signs of inflammation.
Inflammation is the body’s natural protective reaction to injury, infection, or stress. Think of it as your immune system’s alarm system. When something feels off, whether it is too much yeast, an allergen, or even a scratch, the body sends a rapid response team to the scalp. That team brings swelling, redness, itching, and sometimes flaking.
For most people, the reaction calms down after a few hours or days. But if you have a sensitive scalp or a chronic condition, the reaction feels like a fire alarm that never shuts off. It can flare again and again, often without warning. This cycle leaves many people frustrated, embarrassed, and unsure about what to do next.
Myth vs. Fact
-
Myth: “If my scalp is inflamed, it means it is dirty.”
-
Fact: Scalp inflammation is not about hygiene. It is an immune reaction, not a measure of how often you wash your hair.
What are cytokines and why do they matter on the scalp?
Cytokines (pronounced sigh-toe-kynes) are small proteins that act like text messages between immune cells. They do not carry energy or nutrients, they carry instructions. When your scalp senses stress, cytokines deliver the command: “Inflammation needed here.”¹
Some cytokines encourage swelling and heat, which help clear microbes. Others call in reinforcements like white blood cells. Still others calm the storm down when the job is done. Ideally, it is a balanced system. But in sensitive scalps, the messages get out of balance. Too many “attack” signals and not enough “calm down” signals create the burning, itching, or flaking that keeps you up at night.
Here are a few examples of cytokines at work on the scalp:
-
IL-1 (Interleukin-1): Jump-starts inflammation and recruits immune cells.
-
TNF-α (Tumor necrosis factor-alpha): A powerful amplifier that makes inflammation stronger².
-
IL-6 (Interleukin-6): Stimulates both inflammation and tissue repair.
Together, these proteins form a chorus. When they are in harmony, your scalp feels fine. When they are out of sync, the result is irritation.
How local immune activation works in the scalp
The scalp is unique compared to other skin areas because of its density of hair follicles and oil glands. These structures give it natural resilience, but they also create opportunities for immune overactivity.
Here is what happens step by step:
-
Trigger recognition: Specialized cells like keratinocytes (skin cells) and dendritic cells (immune sentinels) recognize stressors such as yeast, bacteria, or allergens.
-
Cytokine release: These cells secrete cytokines into the scalp tissue.
-
Immune recruitment: White blood cells, particularly neutrophils and T-cells, arrive to fight what they perceive as a threat.
-
Symptoms appear: The skin looks red and feels itchy, tight, or sore.
In chronic conditions, the trigger can be very small, or even absent, yet the cycle continues. That is why some people develop flare-ups even when they have not changed shampoo or diet.
Tip for Readers: Keep a simple scalp diary. Write down flare-ups and possible triggers like new products, weather changes, or stress levels. Over time, patterns often emerge.
Which pathways are most important in scalp inflammation?
Scientists have mapped out several “immune highways” that lead to scalp irritation. Each one is driven by a set of cytokines:
-
IL-17 and IL-23 axis: This pathway is central in psoriasis, causing overproduction of skin cells and thick scales³.
-
IL-4 and IL-13: These are classic allergy-related cytokines. They dominate in eczema and lead to extreme itchiness⁴.
-
TNF-α: Acts as a master switch for inflammation. High levels are found in seborrheic dermatitis and folliculitis⁵.
These pathways overlap, which is why scalp conditions can look similar even when the root causes differ. That is also why a “one-size-fits-all” shampoo rarely works for every person.
How does this connect to scalp conditions you may know?
Understanding immune pathways makes it easier to see why certain conditions behave the way they do.
-
Seborrheic dermatitis (dandruff): Triggered by Malassezia yeast, which irritates the immune system. TNF-α fuels flaking and redness.
-
Psoriasis: A chronic condition driven by the IL-17/IL-23 pathway. The body makes new skin cells too quickly, leading to thick scales.
-
Atopic dermatitis (eczema): Dominated by IL-4 and IL-13. It often appears with intense itching and oozing.
-
Folliculitis: Usually bacterial. Cytokines draw neutrophils to hair follicles, creating small red or pus-filled bumps.
Myth vs. Fact
-
Myth: “All scalp flaking is dandruff.”
-
Fact: Flaking can also mean psoriasis or eczema. The treatment approach depends on the underlying pathway, not just the appearance.
What treatments target inflammatory pathways?
Different treatments work by quieting different cytokine pathways:
Medical care
-
Topical corticosteroids: Reduce cytokine activity. They are effective but should not be used for long periods without guidance.
-
Antifungal shampoos: Target yeast in seborrheic dermatitis, lowering cytokine triggers.
-
Calcineurin inhibitors (like tacrolimus): Used in eczema when steroids are not suitable.
-
Biologics: Advanced medicines for psoriasis and eczema that block IL-17, IL-23, or IL-4 pathways.
At-home strategies
-
Wash with lukewarm water, not hot. Heat worsens cytokine release.
-
Pick fragrance-free, pH-balanced shampoos. Harsh detergents can act as triggers.
-
Avoid scratching. Instead, use a cold compress to numb itching.
When should you see a dermatologist?
You do not need to see a doctor for every mild itch. But persistent, painful, or fast-spreading irritation is a signal that professional help is needed.
See a dermatologist if:
-
Symptoms last more than 2–3 weeks.
-
Flakes become thick plaques.
-
You notice hair shedding or thinning.
-
Pain, bleeding, or infection develops.
Dermatologists can order tests, examine skin samples, and recommend treatments that specifically target your cytokine pathways.
Key takeaways for sensitive scalps
Inflammation is not your fault. It is your immune system trying to protect you, but sometimes it overshoots. By understanding cytokines, you gain insight into why flare-ups happen and what helps calm them down.
Remember:
-
Scalp inflammation is driven by immune messengers called cytokines.
-
Different pathways explain why dandruff, eczema, psoriasis, and folliculitis behave differently.
-
Both medical treatments and gentle at-home strategies can restore comfort.
-
Seeking early care helps prevent damage to hair follicles and improves long-term scalp health.
You do not have to live with constant itching or embarrassment. The scalp has an incredible ability to heal when given the right support.
Glossary
-
Cytokines: Proteins that signal immune responses, driving inflammation or healing.
-
Keratinocytes: Skin cells that act as first responders in immune defense.
-
Dendritic cells: Immune cells that detect and present threats to other immune players.
-
IL-17/IL-23 axis: A pathway driving psoriasis-related inflammation.
-
TNF-α: A cytokine central to many scalp inflammatory disorders.
-
Seborrheic dermatitis: A scalp condition causing flaking and redness, often linked to yeast.
-
Biologic therapies: Advanced drugs that block specific immune pathways.
-
Barrier repair: Restoring the scalp’s protective layer to reduce irritation.
-
Calcineurin inhibitors: Non-steroid medicines that reduce inflammation in eczema.
-
Neutrophils: White blood cells that fight bacteria and create pus.
Claims Registry
| Citation # | Claim(s) supported | Source | Anchor extract | Notes |
|---|---|---|---|---|
| ¹ | Cytokines act as immune messengers | Abbas, Cellular and Molecular Immunology, 2022 | “Cytokines act as messengers to recruit immune cells.” | Standard immunology text, authoritative. |
| ² | IL-1 and TNF-α recruit white blood cells | Dinarello, Cytokine, 2018 | “IL-1 is a key recruiter of neutrophils.” | Expert cytokine review. |
| ³ | IL-17/IL-23 pathway in psoriasis | Blauvelt & Chiricozzi, NEJM, 2018 | “IL-23/IL-17 axis drives psoriasis pathogenesis.” | Landmark psoriasis pathway review. |
| ⁴ | IL-4 and IL-13 in eczema | Bieber, NEJM, 2022 | “Type 2 cytokines IL-4 and IL-13 underlie atopic dermatitis.” | Gold-standard atopic dermatitis review. |
| ⁵ | TNF-α in seborrheic dermatitis | Naldi & Rebora, Lancet, 2009 | “TNF-alpha plays a role in seborrheic dermatitis.” | Peer-reviewed dermatology review. |




