Phototherapy for Scalp Psoriasis: Implementation Checklist
Michele Marchand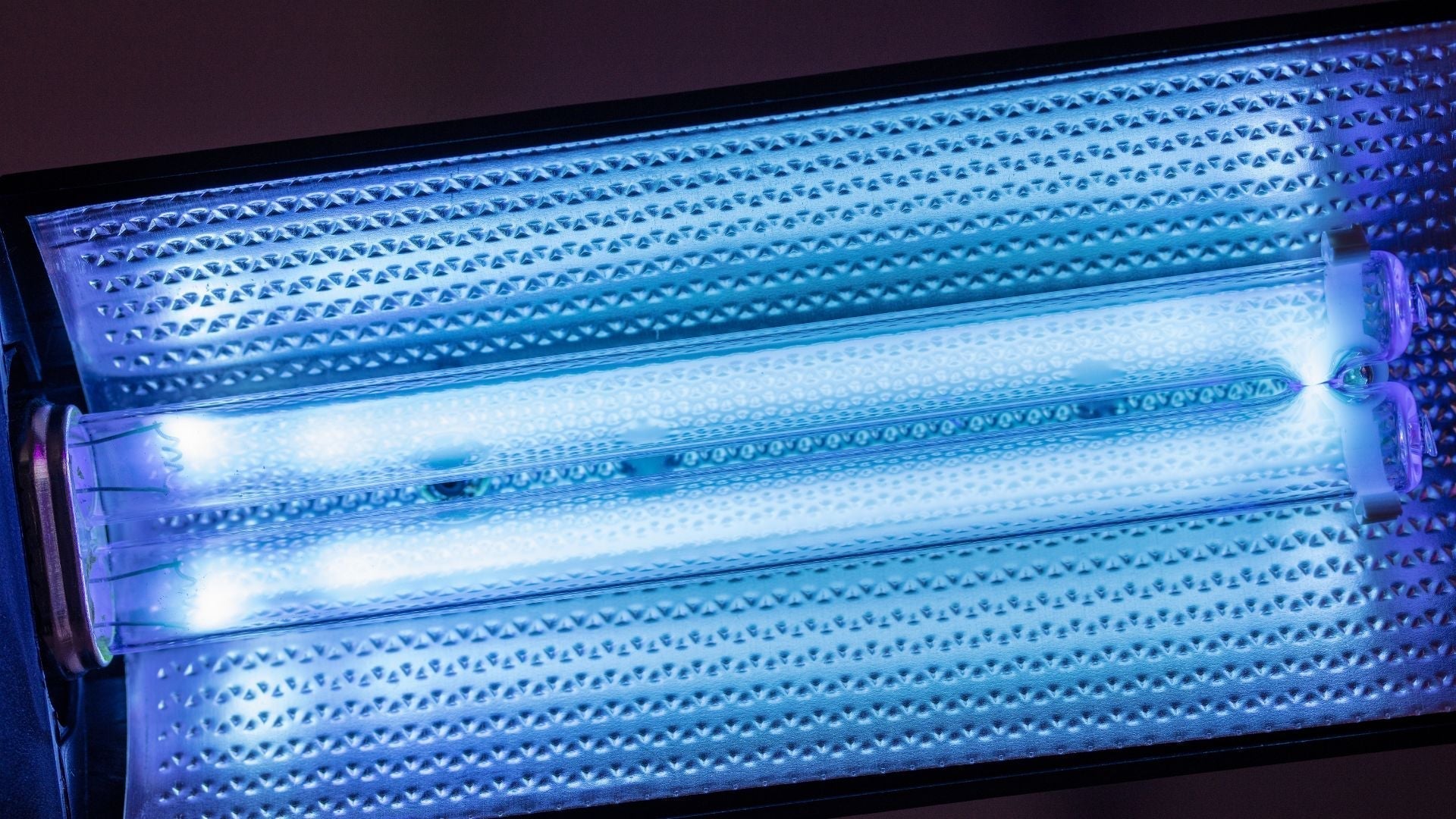
How do you safely use NB-UVB phototherapy at home for scalp psoriasis?
Table of Contents
- What is phototherapy for scalp psoriasis?
- Why is NB-UVB recommended for scalp psoriasis?
- What equipment is used for scalp phototherapy?
- How do you prepare before starting NB-UVB?
- How is dosing calculated for NB-UVB phototherapy?
- What shielding and safety steps are necessary?
- What are the risks of NB-UVB scalp therapy?
- At-home vs. in-clinic phototherapy: which is better?
- Implementation checklist for safe use
- When should you stop or adjust treatment?
- Final encouragement
What is phototherapy for scalp psoriasis?
Phototherapy is a medical treatment that uses carefully measured ultraviolet (UV) light to reduce inflammation and slow the overproduction of skin cells. In psoriasis, skin cells grow and shed too quickly, creating thick, scaly plaques. When this process occurs on the scalp, it can cause itching, redness, and discomfort that interfere with daily life. Creams and medicated shampoos often struggle to penetrate through dense hair, leaving patients feeling frustrated and stuck. Phototherapy offers a way forward.
Narrowband UVB (NB-UVB) is the most widely used form of phototherapy today. Unlike older methods that used a wide range of UV wavelengths, NB-UVB delivers a very specific light spectrum between 311–313 nanometers. Research shows this narrow range is both effective and relatively safe compared to earlier forms of UV therapy¹. For scalp psoriasis, NB-UVB can be administered through specialized comb devices or light units designed to reach the skin beneath the hair, offering treatment without the need to shave.
Why is NB-UVB recommended for scalp psoriasis?
NB-UVB has become the gold standard for light-based psoriasis therapy because it balances effectiveness with safety. Studies have consistently demonstrated that this wavelength reduces redness, scaling, and itching in psoriasis plaques². Unlike systemic medications such as methotrexate or biologics, NB-UVB does not alter the immune system in the entire body. Instead, it targets the skin directly, lowering the risk of systemic side effects.
The therapeutic effect comes from NB-UVB’s ability to calm overactive immune cells that drive psoriasis. It also slows the rapid skin turnover that leads to thick scaling. For many patients, the improvement is gradual. A typical course requires multiple sessions each week, often for several months, before significant changes are visible³. While this may feel like a commitment, the benefit is that once plaques begin to respond, maintenance therapy can often be done at longer intervals, reducing treatment burden.
What equipment is used for scalp phototherapy?
Specialized devices make scalp phototherapy possible even for patients with thick or long hair. These tools are designed to separate hair and ensure UV light reaches the skin:
-
Hand-held NB-UVB combs: These are small, portable units with built-in plastic teeth that lift and part the hair. They allow patients to target specific patches on the scalp, making them particularly useful for at-home treatment.
-
Clinical NB-UVB booths with scalp attachments: In medical offices, larger light boxes may be used, sometimes with attachments or caps that concentrate light on the scalp. These provide stronger, more even exposure and are ideal for widespread or stubborn disease.
-
Targeted excimer devices: Excimer lasers and lamps deliver a concentrated UVB beam directly to plaques. This option is often chosen for small but resistant areas that do not respond to standard NB-UVB.
The right equipment depends on the severity of scalp psoriasis, hair density, and whether the patient is receiving care in a clinic or managing treatment at home. A dermatologist typically guides this choice, ensuring the setup matches individual needs.
How do you prepare before starting NB-UVB?
Preparation is critical for both safety and success. The steps below help patients maximize benefit while reducing risks:
-
Consultation with a dermatologist: Before beginning any phototherapy, a dermatologist confirms the diagnosis, rules out look-alike conditions, and reviews whether NB-UVB is suitable. Certain patients, such as those with a history of skin cancer, may need alternative therapies.
-
Baseline skin assessment: The dermatologist examines skin type, plaque severity, and overall distribution of psoriasis. This evaluation informs how the initial dose is set.
-
Patch test: Sometimes a small test dose of UV light is applied to the skin to gauge sensitivity. This prevents accidental overdosing during the first full session.
-
Medication review: Some drugs increase sensitivity to UV light. These include certain antibiotics, diuretics, and chemotherapy drugs. A thorough review helps prevent harmful interactions.
-
Protective planning: Patients learn how to use protective goggles and shielding before the first session. Proper preparation makes each treatment safer and less stressful.
How is dosing calculated for NB-UVB phototherapy?
NB-UVB dosing is highly individualized. Dermatologists take several factors into account:
-
Initial dose: Usually calculated as 50–70% of the minimal erythema dose (MED). MED is defined as the smallest dose of UV light that causes a faint redness after 24 hours⁴.
-
Incremental increases: If the skin tolerates the initial dose well, the exposure may be increased by 10–20% per session. This gradual rise prevents burns while allowing steady therapeutic progress.
-
Frequency: Most patients are scheduled for 2–3 sessions per week, with at least 24 hours of recovery between them. More frequent sessions do not necessarily speed results and may increase risk.
-
Maximum dose: Different body areas tolerate different levels of UV light. The scalp, which has thicker skin than the face, can usually handle higher doses. Still, upper limits are always set by the dermatologist.
Home devices often come with manufacturer instructions, but safe adjustments should only be made under medical supervision. Overexposure, even in small amounts, can lead to burns and setbacks.
What shielding and safety steps are necessary?
While NB-UVB is considered safe, protective measures are essential every time. Following them consistently prevents side effects and long-term risks:
-
Eye protection: UV-blocking goggles are mandatory during every session. Even a brief glance at the light source without goggles can damage the eyes.
-
Face and unaffected skin coverage: Towels, caps, or protective clothing help shield areas not being treated. This reduces unnecessary UV exposure.
-
Sensitive zones: The lips, genitals, and moles should always be covered. These areas are particularly vulnerable to UV damage.
-
Hair parting: Phototherapy devices are most effective when the hair is moved aside. Using the comb attachment or manually parting hair ensures plaques get full exposure.
-
Moisturizers: It is best to apply fragrance-free emollients after sessions, not before. Pre-session application can scatter the light and reduce effectiveness.
-
Session timing: Each exposure is kept brief, often just a few minutes. Using timers or written logs helps patients track duration and prevent accidental overexposure.
What are the risks of NB-UVB scalp therapy?
Like any medical treatment, NB-UVB carries risks. The good news is that most are minor and manageable:
-
Short-term risks: Redness, mild burning, itching, or dryness may occur in the hours following treatment. These effects usually resolve with moisturizers or spacing out sessions.
-
Medium-term risks: In some cases, uneven exposure can lead to temporary hair discoloration or fragile strands. This risk is higher if the light is not evenly distributed across the scalp.
-
Long-term risks: Prolonged use of UV therapy carries a slightly increased risk of skin cancer. However, NB-UVB’s risk is significantly lower compared to older PUVA therapy, which combined UVA light with a sensitizing medication⁵.
By keeping a regular schedule of dermatology visits and reporting new skin changes, patients can catch potential issues early and continue therapy safely.
At-home vs. in-clinic phototherapy: which is better?
Patients often wonder whether to invest in a home device or stick with supervised clinic sessions. Both approaches have strengths:
At-home devices
-
Provide flexibility and convenience, especially for patients with busy schedules.
-
Allow treatment in privacy without frequent travel to a clinic.
-
Represent a cost-effective solution over time for mild-to-moderate cases.
In-clinic treatment
-
Offers professional oversight, ensuring every dose is accurate and safe.
-
Provides access to more powerful, full-body equipment.
-
Is best suited for patients with severe or treatment-resistant psoriasis who need close monitoring.
In many cases, patients begin with clinic-based therapy to stabilize their psoriasis and later transition to home devices for maintenance. This blended approach combines safety with convenience.
Implementation checklist for safe use
A structured routine helps patients get the best results while minimizing mistakes. This checklist can be followed before, during, and after each session:
Before each session
-
Remove all cosmetic products, oils, or medicated shampoos from the scalp.
-
Put on protective goggles to shield eyes.
-
Cover unaffected skin with cloth barriers or sunscreen.
-
Carefully part hair to make plaques accessible.
During each session
-
Hold the device close to the scalp, without pressing too hard.
-
Treat each affected zone for the prescribed amount of time.
-
Keep a written or digital log of exposure times for consistency.
After each session
-
Apply a fragrance-free moisturizer to soothe the scalp.
-
Check for redness, burning, or irritation.
-
Contact a dermatologist if reactions are severe or persistent.
When should you stop or adjust treatment?
Sometimes phototherapy needs to be paused or adjusted. Stop treatment and consult a dermatologist if you notice:
-
Painful burning or blistering that does not resolve quickly.
-
Worsening psoriasis or spreading lesions.
-
Signs of infection such as swelling, pus, or warmth in treated areas.
Dermatologists typically evaluate progress after 8–12 weeks. If plaques improve, sessions may be tapered to once weekly or biweekly for maintenance. If little improvement occurs after 3–4 months, the dermatologist may recommend alternative therapies, including systemic medications or biologics.
Final encouragement
Living with scalp psoriasis can feel discouraging, but NB-UVB phototherapy provides a safe, well-researched treatment option for those who struggle with topical solutions. With proper setup, consistent dosing, and safety measures, many patients see significant relief from itching, scaling, and redness. The most important step is partnering with a dermatologist to create a plan tailored to your skin. With time, persistence, and professional support, phototherapy can transform how you manage your scalp health.
Glossary
-
Phototherapy: Medical treatment using ultraviolet (UV) light to improve skin conditions such as psoriasis.
-
NB-UVB (Narrowband UVB): Specific wavelength of UV light (311–313 nm) proven effective for psoriasis.
-
Psoriasis plaques: Thick, raised patches of inflamed skin covered with silvery-white scales.
-
Minimal erythema dose (MED): The lowest UV dose that produces faint redness after 24 hours.
-
Fitzpatrick skin type: Classification of skin’s response to sun exposure, ranging from type I (very fair) to type VI (deeply pigmented).
-
Excimer device: A machine delivering concentrated UV light to small, resistant skin patches.
-
Emollient: Moisturizer that softens, hydrates, and protects the skin barrier.
-
PUVA therapy: An older phototherapy combining psoralen (a drug) with UVA light, associated with higher risks.
Claims Registry
| Citation # | Claim(s) supported | Source title + authors + year + venue | Anchor extract | Notes |
|---|---|---|---|---|
| 1 | NB-UVB (311–313 nm) is effective and safer than broad UV therapy. | Elmets CA, et al. "Phototherapy and photochemotherapy of skin disease". J Am Acad Dermatol. 2014. | "Narrowband UVB (311–313 nm) is the most effective and safest form of UVB." | Authoritative dermatology guideline. |
| 2 | NB-UVB reduces itching, redness, and scaling while minimizing risks. | Menter A, et al. "Guidelines of care for the management of psoriasis". J Am Acad Dermatol. 2009. | "NB-UVB is highly effective and well tolerated in the treatment of psoriasis." | Widely cited U.S. guideline. |
| 3 | Multiple sessions per week for several months are needed for improvement. | Yones SS, et al. "Randomized controlled trial of NB-UVB vs PUVA". Arch Dermatol. 2007. | "Patients required an average of 20–30 treatments over 8–12 weeks." | Clinical trial data. |
| 4 | Initial NB-UVB dose set at 50–70% of minimal erythema dose (MED). | Garritsen FM, et al. "Phototherapy in the era of biologics". J Eur Acad Dermatol Venereol. 2016. | "Starting dose is typically 50–70% of the MED." | Clinical review article. |
| 5 | Long-term risks include slightly increased cancer risk, but lower than PUVA. | Archier E, et al. "Carcinogenic risks of phototherapy". J Eur Acad Dermatol Venereol. 2012. | "NB-UVB carries a lower carcinogenic risk than PUVA." | Meta-analysis of cancer risk. |




